Ep. 336 Lipid Masterclass: An Introduction to Lipids and Cholesterol with Dr. Thomas Dayspring
- February 17, 2024
- No Responses
Today, I am excited to share the first class in a series of lipid masterclasses with the amazing Dr. Thomas Dayspring!
Dr. Dayspring is certified in internal medicine and clinical epidemiology and is a fellow of the American College of Physicians and the National Lipid Association. He was previously the Educational Director of a nonprofit organization and has served as the Chief Academic Advisor for two major cardiovascular labs.
Due to the in-depth nature of my discussions with Dr. Dayspring over several sessions, each lasting nearly six hours, it seemed logical to present these masterclasses in segmented chunks to make them easier to understand.
In our first class today, we dive into the fundamentals, exploring what lipids are and how lipids and fatty acids are classified. We cover the physiology and transportation of cholesterol and the role of apoptosis, apo-proteins, and apo-lipoproteins, unravel the differences between HDL, LDL, IDL, and VLDL, and explain how to calculate LDLs and triglycerides for assessing metabolic health. Dr. Dayspring also shares his preferences regarding lab values and the indicators that provide information to help him determine the early risk of cardiovascular disease.
We get into some detailed aspects of physical chemistry in this episode, so I highlight the main clinical points throughout our conversation to make it more understandable.
Be sure to join Dr. Dayspring and me for our next episode in the lipid masterclass series.
“Cholesterol is one of the lipids that is crucial for human life in certain amounts. Beyond that, it can cause harm.”
– Dr. Thomas Dayspring
IN THIS EPISODE YOU WILL LEARN:
- What are lipids, and why are they important?
- Dr. Dayspring explains what triglycerides are.
- How lipids get absorbed and transported throughout the body
- What lipoproteins are, and how they get classified
- How cholesterols get calculated
- The impact of triglycerides on cholesterol levels and cardiovascular health
- How high triglyceride levels can indicate early insulin resistance or increased ASCVD risk
- What is the role of HDL particles?
- How metabolic syndrome impacts cardiovascular health
Bio:
Thomas Dayspring MD is a Fellow of both the American College of Physicians and the National Lipid Association and is certified in internal medicine and clinical lipidology. After practicing in New Jersey for 37 years, in 2012, he moved to Virginia. He served as an educational director for a nonprofit cardiovascular foundation and until mid-2019 as a Chief Academic Advisor for two major CV laboratories. Since then, he has served as a virtual cardiovascular / lipidology educator. Career-wise he has given over 4000 domestic (in all 50 states) and several international lectures, including over 600 CME programs on atherothrombosis, lipids/lipoproteins (and their treatment), vascular biology, biomarker testing, and women’s cardiovascular issues. He has authored several manuscripts and lipid textbook chapters and performed several podcasts. For several years he was an Associate Editor of the Journal of Clinical Lipidology. He was the recipient of the 2011 National Lipid Association’s Presidents Award for services to clinical lipidology and the 2023 Foundation of NLA Clinician/Educator Award. He has over 34K followers on his educational Twitter (X) feed (@Drlipid). He has Gold Heart Member status as a professional member of the American Heart Association and serves as a Social Media Ambassador for the European Atherosclerosis Society and the National Lipid Association.
Connect with Cynthia Thurlow
- Check out Cynthia’s website
- Submit your questions to support@cynthiathurlow.com
Connect with Dr. Thomas Dayspring
Images from Dr. Thomas Dayspring:
Transcript
Cynthia Thurlow: [00:00:02] Welcome to Everyday Wellness podcast. I’m your host, Nurse Practitioner, Cynthia Thurlow. This podcast is designed to educate, empower, and inspire you to achieve your health and wellness goals. My goal and intent is to provide you with the best content and conversations from leaders in the health and wellness industry each week and impact over a million lives.
[00:00:29] This episode of Everyday Wellness is the first in a series of Lipid Masterclasses with the incredible Dr. Thomas Dayspring, who is a fellow of both the American College of Physicians and the National Lipid Association and is certified Internal Medicine and Clinical Lipidology. He has served as Educational Director for nonprofits and has previously served as a Chief Academic Advisor for two major cardiovascular labs. He is an absolute delight. And because of the in-depth conversation that Dr. Dayspring and I have had over a series of multiple conversations nearly 6 hours in length, it made the most sense to break these lipid masterclasses into chunks to make it easier to understand. If you are listening right now, you may want to go back and dog tag this podcast episode and listen to it several times.
[00:01:30] In this first episode, we discuss what are lipids? The classification of lipids and fatty acids, the physiology of cholesterol, as well as transportation, the role of apoptosis, apo-proteins and apolipoproteins, differences between HDL, LDL, IDL, and VLDL. How to calculate LDLs and triglycerides? Looking at clues for poor metabolic health, his preferences in terms of lab values, and clues to determine or to provide information about early cardiovascular disease risk. This episode is a bit heavy and physical chemistry. However, I do make sure, as I’m weaving through the conversation, I’m picking up the clinical pearls to make it easier to understand. Again, this is a first masterclass in a series. Stay tuned for the rest. I’m really excited you’re joining us.
[00:02:35] Welcome, Dr. Dayspring. I’m so grateful and so appreciative of the work that you do and really excited to introduce you to my Everyday Wellness community.
Dr. Thomas Dayspring: [00:02:44] Well, I’m very happy to be here, Cynthia. And, you know, it’s so funny because we contacted each other without really knowing too much about each other, and lo and behold, we’re actually probably within 10 miles of each other where we live in Central Virginia. So even though this is a virtual podcast, I could have easily driven down to your studio and looked at you in person. So, this should be a lot of fun.
Cynthia Thurlow: [00:03:07] Absolutely. Absolutely, and to give listeners some context to the topics we’re going to be exploring today. Let’s talk a little bit about basics, lipid biology. What exactly are lipids? Why are they important? Because I think over the past 50 or 60 years, there’s been a lot of emphasis on fearing the role of cholesterol. But cholesterol is very important in the body. And I know you are an expert in talking about lipids and
and lipidology. So, let’s start with the basics to kind of give our listeners and our community some context to some of the discussions that we’re going to have today and moving forward.
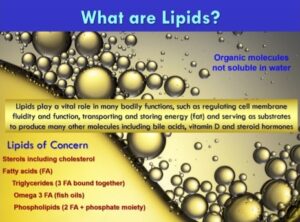
Dr. Thomas Dayspring: [00:03:44] Sure. Well, the first thing is absolutely to define what the heck is a lipid. Biochemistry is full of a lot of molecules, all of which perform various functions or so, and many of them in the animal kingdom. And certainly, cholesterol is one of the lipids that is absolutely crucial for human life in certain amounts. Beyond that, it can cause harm, too low it can cause harm. So, lipids are basically oils. And what that means is they are molecular compounds that are not soluble in water. Everybody knows, pour some olive oil in a glass of water and it’s not missable, it doesn’t circulate, it floats on top. So, this does create certain physical chemistry attributes in the human body, because lipids have to traffic from one cell to another.
[00:04:33] And the only way lipids traffic is in our bloodstream, our plasma, which happens to be what scientists would call an aqueous solution, meaning it’s water. So how in the world do these things that hate water, that’s called hydrophobic molecules lipids, do they circulate in water? So, evolution had to solve that problem and we’ll get into that soon. The lipid category, they’re actually organic molecules, which means they are carbon, hydrogen and oxygen atoms, perhaps with another atom here they’re attached to it, but they’re stuck together in various joint ways of constructing macromolecules, and they form this whole class of lipid molecules. The lipids that are most talked about by laymen when they see their doctors or by physicians or clinicians like yourself, are cholesterol of course. But cholesterol is just one of many other sterols. So, sterols are a big classification of lipids.
[00:05:37] Cholesterol is obviously talked about the most, but there are 40 or 50 other ones. All of those other ones are grouped in a name called noncholesterol sterols. I prefer the term xenosterols. Xeno means other in Greek. So other sterols that are not cholesterol, and believe it or not, they play big roles also in the human body. And it’s not only the animal kingdom that has cholesterol and other sterols in it, but the plant kingdom does also. And most of the sterols that are in plants are not cholesterol. That’s pretty much in the animal kingdom. We call that a zoosterol. And of course, the sterols that are in plants are called phytosterols. No surprise. So, we have cholesterol, bunch of other sterols, and you got a big grouping called phytosterols. The other lipids of course of interest to everyone, including clinicians, are fatty acids. And fatty acids are also crucial for human life.
[00:06:36] The good news is, other than two or three of them, the human body can de novo synthesis all of the fatty acids it may need, or so. So, there’s only a couple of essential fatty acids that you have to eat that the body would have very tough trouble to synthesize. And there, as you know, the omega-3 class of fatty acids or so I’m sure sooner or later we’ll touch on them. The other fatty acids are important because we eat them, they get absorbed, and they’re then used again. Many of the fatty acids, the one that mostly affects cardiology and atherosclerotic risk, are fatty acids, to just create efficiency, are traffic bound together. So, if I take a backbone molecule that can attach two fatty acids and that’s called glycerol. Glycerol is a 3 carbon sugar. One, you’d see 3-carbons and of course you can stick things onto those carbons.
[00:07:34] So, if I stuck two fatty acids onto a glycerol molecule and I stuck another molecule that has a phosphorus moiety in it, I just created a phospholipid. Phospholipids are two fatty acids on glycerol with a head group that has phosphorus in it. And there are many of those head groups super crucial to the human body, because phospholipids make up virtually all of our cell membranes and they contribute to the functionality of our cells. That means are we going to have healthy cells or not so healthy cells? And the phospholipid construction has everything to do with that. And most important to the phospholipids are which fatty acids are stuck in them and which phosphorus head group is on them too. Phospholipids are the lipid molecules that are least understood in the clinical community. Unless you go into advanced lipidology, they’re not talked a lot about. And the reason why is we don’t typically measure phospholipids in the bloodstream when we do lipid analyses on people. But you’ll hear me talk about them because they are kind of super crucial to where I’m going.
[00:08:42] And of course, the last lipid molecule and everybody knows about this. In the dark ages, it was dismissed as, “Oh, that’s not important.” And nowadays, in our little insulin resistant world, it’s become a crucial lipid. So, if I take that glycerol molecule with 3 carbons and I stick three fatty acids on it, the biochemical name for a fatty acid is acyl. So, if I took three acyl groups, three fatty acids, and stuck it on a glycerol molecule, I would have triacylglycerol, better known to the world as triglycerides. It’s funny, when I started back in the dark ages [chuckles] in the 1960s, they were just simply called glycerides. And the term triglycerides evolved as well. A diglyceride is really a phospholipid and a triglyceride is a way for three fatty acids to get in.
[00:09:32] Now, most of the fats that we eat, animal fats, are in the form of a triglyceride. So, we chew, maybe it’s a piece of meat, maybe it’s whatever, and in come those triglyceride molecules, they are pretty monstrous molecules with glycerol and three, many, oftentimes long chain fatty acids stuck onto them. So, they are unabsorbable. And evolution had to figure, “Oh, my God, we got to get these fatty acids into the body. Some of them are important, especially those omegas.” And so were given a pancreas, and pancreas, when we eat, our body signals the pancreas, “Hey, shoot out some enzymes. The gut is going to need to dissolve certain macromolecules that we eat so they can be absorbed.” So the pancreas shoots out a whole class of enzyme called lipases. Lipases dissolve fatty acids from glycerol. We have phospholipases that digest eaten phospholipids, and we have triglyceride lipase, lipoprotein lipase, whatever you want to call it, intestinal lipase.
[00:10:36] And what that does, as we swallow those big three fatty acids on a glycerol, it starts cleaving the fatty acids off of the glycerol. So now simple fatty acids are easily absorbed by intestine. And the intestine has a membrane transporter that recognizes the fatty acids and pulls them into your intestinal cells. Likewise, most of the cholesterol we eat is also in an esterified form, which means, yes, it’s a cholesterol molecule, but it’s bound to usually a long chain fatty acid that’s called cholesteryl ester. If you listen to my pronunciations, cholesteryl ester Y-L, not O-L, esters have Y-L is the biochemistry abbreviation. So, if we swallow this big monstrous cholesteryl ester molecule, the pancreas shoots out a cholesteryl esterase, another lipase, and it cleaves the fatty acid off of the cholesterol. And what you have in your intestinal lumen now is called free cholesterol and that is easily absorbed.
[00:11:37] There’s a specific transporter looking to bind to cholesterol, and it’ll pull it in. Just an aside, the receptor that pulls in cholesterol is a very different receptor than what pulls in fatty acids. Ergo, absorption of cholesterol has nothing to do with absorption of fatty acids. But always lipids get into our enter sites. But we’re a complicated little machine, including our intestine. So that was a long answer on what the heck lipids are. I’ve given you the major classes that I’m sure we’re going to elucidate more about, or so, but they’re just little oily molecules that I showed you how they get in. And now once they get into the intestine or if cells are making them, how in the world do they jump from one cell to another in the plasma? So I’ll stop there, unless you want me to answer that question or you can point me in another direction.
Cynthia Thurlow: [00:12:27] No, you did a beautiful job. And I think for so many listeners, this might be the first time that they’re hearing how this process works. I think that there’s this presumption that we chew food, we swallow it, and then it instantaneously, magically gets to where it needs to be. So, this explains why individuals that are lacking lipase, or perhaps their body’s not making as much, can contribute to fat malabsorption and clinically, some of the issues that we see. So, we talked about a little bit about lipid biology. Let’s talk about how these lipoproteins actually move, these little transportation vehicles that we have in the body.
[00:13:05] And I love the analogies to thinking about them like machinery or cars, because it helps people understand, because these can be some complicated concepts helping people understand that lipids and proteins, how they get around the body to where they need to be. You mentioned they’re absorbed into the gut lumen with specific enzymes and carrier molecules. But let’s talk a little bit more about how we go from talking about phospholipids, phospholipid bilayers, triglycerides, esters, etc. Until we’re actually talking about the transportation system in the body.
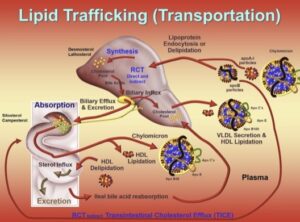
Dr. Thomas Dayspring: [00:13:36] Yup. So basically, I’ve led in this journey we’re going that you got these lipid molecules floating in your intestine. If the pancreas has done the proper enzymes, you have a lot of lipid molecules that the body has to make a decision, should I absorb them or should I not? And obviously, it’s always going to absorb X amount, hopefully not over absorb, but unfortunately that can happen. Or hopefully not under absorb, because as you sort of use the word malabsorption, you don’t want to under absorb lipids or that might cause some problems. So basically, I told you how some lipid molecules get into the intestinal cells. They’re called enterocytes. They line the intestine. But so, what? They’re in cells. What if another cell in the body needs some of those fatty acids or the cholesterol you just absorbed? How in the world do they get there? So, one little aside before I answer that magical question is, of course, every cell in the body can certainly make all the cholesterol it needs. There is no cell that actually constantly requires a supply of cholesterol to get it to it.
[00:14:46] Now, I mentioned phospholipids are so crucial because they line every cell membrane, but not by themselves. In betwixt phospholipid molecules is another essential lipid that makes the cell membrane totally functional. And guess what, it’s cholesterol. So, your cell membranes not only need phospholipids, they need cholesterol a certain amount in betwixt the phospholipids. And if we all have the right type of phospholipids aligned on the surface of our cells and there are interspace cholesterol molecules, we will have functional cell membranes. And what functional means is the membrane allows certain receptors to be placed strategically in the membrane. And those receptors can either pull in substances that the cell needs or if the cell has some garbage, these transporters on the membrane can evict stuff that the cell wants to get rid of. But of course, if it evicts it’s got to put it in something. It doesn’t just dump it into our bloodstream. So that’s the phospholipid cholesterol cell membrane story.
[00:15:55] One thing, just for accuracy, you did mention the word bilayer. What that means is think of the cell as a balloon, so on the surface is all these phospholipid molecules, but they’re aligned. There’s an outer layer that interfaces with the water in the plasma, and then they join another layer of phospholipids, and it’s the fatty acid tails that interlock with each other. So, the outside of the phospholipid membrane is partially water soluble. That’s the phosphorus moiety. And then the inside has also got the phosphorus moiety because it interacts with the cytosol of the cell, which is pretty much another aqueous milieu also. So, bilayer of phospholipids with intermixed cholesterol molecules, and hopefully you got the essential phospholipids and the right amount of cholesterol.
[00:16:48] Now, I did mention cholesterol is necessary for human life. Absolutely, you got to have X amount. Each cell has to have X amount of cholesterol because that’s how it gets in the cell membrane. The cell makes it, and it just translocates through the cytosol and jumps into the membrane. All right, but what happens if, for some reason, there’s the wrong type of substrates in that cell and it overproduces cholesterol? It’s got more cholesterol molecules than it needs. Cholesterol in physiologic amounts is, “Thank you, Jesus, we need that for normal function.” But excess cholesterol is incredibly toxic. It crystallizes and it kills the cells. The medical term for that is apoptosis. You really don’t want your cells dying prematurely. So, the last thing you want in any cell is excess cellular cholesterol. Good news. Evolution knew that would be a problem. So it said, if any cell has excess cholesterol, we have a cholesterol efflux protein, which the cell can make. It will relocate at the cell membrane, and it will take excess free cholesterol and efflux it out to, uh-oh, you got to have a cholesterol acceptor.
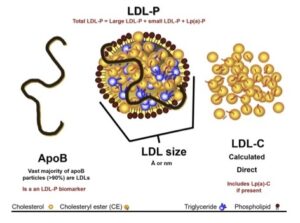
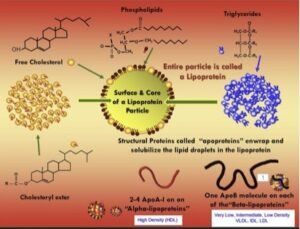
[00:18:00] So here’s how these lipid molecules traffic through plasma. The acceptor molecule for lipids is a protein. You sort of indicated that. Proteins are the carrier for lipids in plasma. Proteins are soluble in an aqueous water medium. So, if our cells got too much lipids, it can evict them, they attach to proteins, and some of the proteins they attach to are big enough to accept several lipid molecules. And once lipids are surrounded by proteins, you have a water-soluble lipid transportation vehicle. Now, I gave you the anatomy of the cell. Let’s take these big– lipoproteins are pretty much circular protein in wrapped molecules. So on the surface, you got the big protein that makes them soluble in water, and then you have a conglomeration of lipids. What is the outer layer of this lipoprotein macromolecule I’m describing? Guess what? It’s phospholipids and free cholesterol, the same thing that lines our cells, except on a lipoprotein it’s a monolayer, it’s not a bilayer.
[00:19:10] So, you have a simple layer of phospholipids and free cholesterol. They have some water solubility, and that’s why they’re on the surface of a lipoprotein. Inside the lipoprotein particle is what we call the core, and that’s where all the water-heating lipids, the hydrophobic lipids, will be carried. And they are cholesterol ester, cholesterol with a fatty acid attached and triglycerides. So now you got this balloon that is water soluble because of its covering of phospholipids and proteins. Inside few of us remember back in probably grammar school or high school, we were taught how to calculate the volume of various shapes. The volume of a sphere, a circular molecule is a third power of the radius. So, it doesn’t take even incredibly minimal changes in the radius, translates in the ability to carry several thousand more lipid molecules. So a third power of the radius.
[00:20:09] I’ll bet most people don’t know it takes 16 marbles to fill a ping pong ball. You would think it would take two or three marbles, but because it’s the third, golf balls are bigger, not that much bigger, but the radius if you do a cube of it, can take a lot more volume. And that’s why when we talk more about these lipoproteins, some of them are really big balloons and some are real tiny. And we’ll explain why evolution made some tiny and some big as we talk more importantly about lipid transportation in the aqueous plasma. So, the protein that accepts cholesterol out of all the cells in our body, exterior to the brain, the brain has its own lipid transportation system, which has almost nothing to do with what’s going on in the plasma. And I hope either in this one or a future podcast, we can spend some time up in our noggins because they’re pretty important, and we’re just basically in our infancy, understanding lipids in the brain. So that is well worth another talk down the road.
[00:21:13] But you got to know the basics before you cross that blood-brain barrier and start seeing what’s going on up there. So, if I’m a cell and I’ve made too much cholesterol and I say, “Oh, my God, I’m going to die unless I can evict it, they upregulate an efflux transporter.” I’ll give you a big name. The abbreviation is ABCA1 transporter, ATP binding cassette transporters. A1 is the one that evicts free cholesterol into certain protein molecules. But there are other members of the ABC family which we don’t have to really expound about now. So too much cholesterol gets evicted by an ABCA1 transporter. And what is the protein that’s accepting cholesterol from cells? These proteins that wrap lipids are called apoproteins and once they accept lipids, they’re called apolipoproteins, and they evolve into the full lipoprotein.
[00:22:09] So the Apoprotein that accepts lipids from our peripheral cells is called apoprotein, capital A-1 either Arabic or Roman number one. ApoA-1 is the structural protein of our high-density lipoproteins, our HDLs. So HDLs are the important lipoproteins that say, “Okay, Mr. Cell, you got too much cholesterol, I’ll take it and I’ll bring it somewhere else to spare you cholesterol toxicity.” So the HDL, when it accepts only free cholesterol, but those phospholipids that line the surface, they carry two fatty acids, don’t they? So, the HDL particle also carries an enzyme. We’ll call it LCAT, [chuckles] because it’s L-C-A-T lecithin cholesterol acyltransferase for the scientists listening to this podcast. So, what that enzyme does is it takes one fatty acid off of the leg of a phospholipid and it attaches it to cholesterol, forming cholesterol with a fatty acid cholesterol ester. That’s an incredibly hydrophobic, water-heating cholesterol molecule.
[00:23:18] So free cholesterol can actually sit on the surface of an HDL. But if it gets a stir fight, it has to migrate to the core of the HDL. So that process keeps occurring and occurring and occurring as the apoA-1 accepts more and more cholesterol. And before you know it, right before our eyes, our HDL particle matures from a little flatbed truck to a discoid truck to a balloon. And that is the mature, fully cholesterol loaded HDL particle, which can float around our plasma because apoA-1 is soluble. Interesting, the HDLs carry 1, 2, 3, 4 or even five molecules of apoA-1. And so, it’s a macromolecule. As we’re going to talk about the whole lipoprotein family, it is by far the smallest compared to the other ones that are floating around. And because it’s small, even though it’s carrying a lot of molecules, by the way, most people are not taught this, and it’s one of these interesting factoids if you ever do medical trivia. How many molecules of cholesterol are actually in each and every mature HDL particle? It’s 45. It doesn’t sound like a lot. And that’s why HDLs are so small. Yes, they carry cholesterol, but because there are quadrillions of HDL particles, doesn’t matter that they’re smaller, like an army of ants that can carry away a lot of stuff, but each one is tiny.
[00:24:43] When we first discovered lipoproteins in the 1940s, the people who did that, did it found separated them in a centrifuge. They took serum and they put it in a centrifuge and spun it around. It was a big, powerful, ultra centrifuge. Centrifuge for over 24 hours and after that, they saw there are distinct layers of lipoprotein particles. So, the first classification is they described them by their density. The ones that floated on top were called very low-density lipoproteins. We know them today as VLDLs. Little sunk into the tube was low-density lipoproteins, and on the bottom of the tube was the high-density lipoproteins. Now, what determines the buoyancy of these particles? It’s like the same thing if you jump in a swimming pool, fat people float more than skinny people who sink to the bottom. So, the HDL carries few lipids. It’s mostly proteins, so it sinks. It has a very high density, hence the name.
[00:25:45] The VLDLs are full of lipids. They’re big fat balloons, so they float. They don’t sink very much at all. And as they lose lipids, they become smaller, so their density gets a little lower because they’re losing lipids, and they become the low-density lipoproteins. I did say, “Hey, lipids get into the intestine.” The intestine does make its own lipoprotein, which takes lipids into our plasma and brings them to certain tissues of the liver. They’re monstrous. The biggest of our lipoproteins, and they’re called chylomicrons, and they basically float in a centrifuge tube. [chuckles] They’re so fat, so full of lipids, they just float. They don’t sink at all. So, we have chylomicrons, very low density, low density and high density. Trivia in between low density and very low density is a transient particle called intermediate density, IDL.
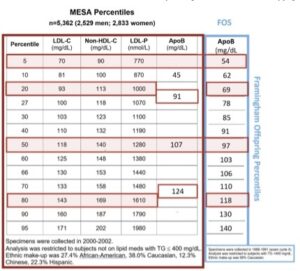
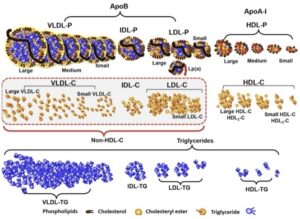
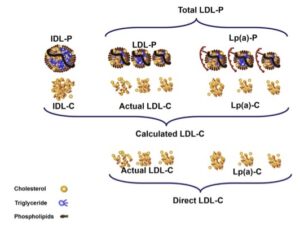
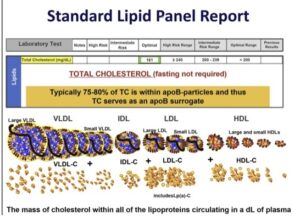
[00:26:42] So I’ve just named all the lipoproteins to you, VLDLs, chylos, IDLs, LDLs, and HDLs. There are no others within each class. Each class is sort of a heterogeneous mixture of particles determined by their buoyancy. The big fat ones, as they lose lipids, become smaller, smaller, smaller. So, as a VLDL loses its lipids, it gets to a point where you can’t call it a VLDL anymore. It becomes an IDL. And the IDL rapidly loses some lipids. And you can’t call it an IDL anymore. It becomes an LDL. That’s our total family of lipoproteins. By the way, we’re going to talk a little bit about measuring lipid metrics in the laboratory. So, usually on the top of every lipid profile a person gets back is something called total cholesterol. Total cholesterol would be the laboratory has separated all of the lipoproteins and it assayed the cholesterol that’s in each and every lipoprotein and added them together, total cholesterol is basically VLDL cholesterol plus IDL cholesterol plus LDL cholesterol plus HDL cholesterol. So that’s your total cholesterol metric.
[00:27:55] We don’t get it in our laboratory reports, but fancy labs could give you a VLDL cholesterol level by assaying the amount of cholesterol and VLDLs. In a little while, I’m going to tell you’re not going to get that reported to you, but it’s an easy calculation if you’d like to do it. Of course, labs report LDL cholesterol to us. Most labs, believe it or not, they don’t directly assay the cholesterol that’s in your LDL particles. There’s another mathematical formula that allows them to guess it. Mathematical formulas are cheaper than buying reagents that can directly measure something. So that’s called a calculated LDL cholesterol as opposed to a directly measured LDL cholesterol, which does cost a little more money because the lab has to buy these assays that just will give us that specific value.
[00:28:46] In general, directly measured and calculated LDL cholesterol in physiologic circumstances have a high degree of accuracy concordance as it’s called. But unfortunately, [chuckles] and another topic we’ll head into, sometimes they are direct LDL cholesterol does not match the calculated. That’s called discordance. And then you have to know, do I believe the calculated, or do I believe the direct? More on that later. And then, of course, all labs directly measure the cholesterol that is in HDLs. So, you have the directly measured HDL and total cholesterol. VLDL cholesterol is a calculation. But if you calculated VLDL cholesterol, now if you took total cholesterol and subtract it from it, your VLDL cholesterol and your HDL cholesterol, you would have your calculated LDL cholesterol level. That’s the formula. It’s that easy.
[00:29:44] And I might as well get to it now, because I want to jump back to the HDLs that have accepted cholesterol from your cell. But the calculation for VLDL cholesterol was discovered in the mid-1970s by one of the gods of lipidology, Dr. Friedewald. And he said, “Listen, VLDLs are mostly triglyceride carrying particles. On average, they carry five times more triglyceride than cholesterol. Almost all of the cholesterol that we measure in plasma is VLDL triglycerides.” So, if I take total triglyceride levels on the assumption that they’re all in VLDL particles, which is not exactly the truth, but we’re talking in general terms here and divided it by five, because there are five times more trigs in cholesterol, I would calculate my VLDL cholesterol. And then I have my equation. Subtract the calculated VLDL cholesterol, the HDL cholesterol from total cholesterol. What’s left? That’s your LDL cholesterol. You could see where that might go wrong. Is your triglyceride measurement too much or too little? As the triglyceride levels go up, up, up, that calculation becomes erroneous, and therefore, your calculated LDL cholesterol becomes erroneous. Let’s get away from clinical chemistry a bit. Unless you want me to elucidate on any of that, because I want to go back to the HDLs.
Cynthia Thurlow: [00:31:08] Yeah. So out of curiosity, you were indicating that as your triglycerides are going up, it lessens the specificity of the calculated LDL. Where in the literature, the research, or your clinical experience, where is that number for triglycerides? Because I know when I was working in cardiology, there were certain numbers and metrics we like to focus in on, and triglycerides obviously were one of them. But in your research and in your experience, what is that number where you feel like it starts to lessen the power of that calculated LDL?
Dr. Thomas Dayspring: [00:31:39] Great question. And listen, when Dr. Friedewald invented the formula, he warned there were shortcomings to it if you read the whole paper, but you remember back in the 1970s, and he’s probably looking at 1960s blood from populations, very different lipid concentrations in those people back then, compared to us 50, 60, 70 years later for goodness sakes. And what happened is we developed insulin resistance in our population, and one of the hallmark lipid abnormalities was raising triglycerides. That’s always a clue to a clinician that you’re dealing with insulin-resistant prediabetic or diabetic. The incidence of all of those are probably five times more than what they were in Dr. Friedewald’s term. Diabetes was there, but it was nowhere near the epidemic that it is now.
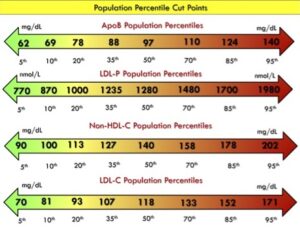
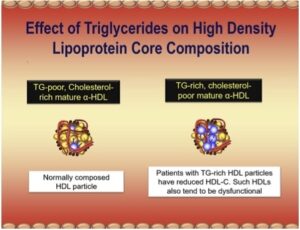
[00:32:31] So, to answer your question, initially they said, “Hey, when the triglycerides hit 400, don’t use that calculation.” There weren’t that many who had triglycerides that were elevated back then. But as guidelines evolved and the first time they started giving us triglyceride numbers that had any accuracy were in the late 90s, around 2000. And they made the declaration that a triglyceride above 150 is high risk triglycerides. That is certainly true. But I would like your audience to know a trig of 150 is the 75th percentile, and that means at a trig of 150, [chuckles] 75% of the population has a triglyceride under 150. And a lot of them are prediabetics and even early diabetics. So obviously a trig of 150 is like burglar alarm, evacuate the building as quickly as possible. [Cynthia laughs] But I would like that burglar alarm to go off when your trigs are around 100, because that is where trigs start getting into lipoproteins that they have no business being in, and they distort whatever those lipoproteins are supposed to be doing. And the particles they get into that they’re not supposed to be in our LDLs and our HDLs and triglyceride starts invading an LDL or an HDL. What gets knocked out? Cholesterol.
[00:33:59] So, as triglycerides goes up, it’s not uncommon to see LDL cholesterol going down. But that’s not a victory. That’s a nightmare. And I’ll explain why. I keep saying I got a lot of stuff to explain later, but same with the HDL. And HDL should in essence carry no triglyceride molecules. But if trigs start sneaking in, and they do have a way of getting in, the HDL garners more and more trigs. We don’t measure HDL triglycerides, but if we did, we would see this. But if trigs invade an HDL, what has to leave? Cholesterol. I think everybody knows as trigs goes up, there’s an inverse relationship with HDL cholesterol, it goes down. Many people use the triglyceride/HDL ratio, and that ratio is basically trigs going up, HDL cholesterol going down. So the ratio goes up, because HDLC is the denominator in that ratio. Dan Rader is the first to describe this, and he used a term which I love, “As trigs invade an HDL.” We should call them fat HDLs, because it’s like obese people. You can see their belly is carrying something it shouldn’t. Well, if trigs invade an HDL, they’re getting fat, and unfortunately, they can’t carry cholesterol, which happens to be the major, one of the big reasons HDL particles exist.
[00:35:20] So, using that, I’m going to jump back. I told you, HDLs accept unwanted cholesterol from cells. They have this enzyme LCAT that esterifies it making the HDL a big balloon full of cholesterol ester. Almost no triglycerides in that molecule, a couple, but nothing of any concern. Now, you have all these big, gigantic HDLs floating around your plasma. Obviously, you have to do something with that cholesterol. They don’t float forever, and they need actually, one of the purposes of HDLs is to bring to cholesterol that was not wanted by cells and bring it to either an organ that can get rid of the excess cholesterol or bring it to some cells that might actually need some extra cholesterol. So here are the avenues for mature HDL particles.
[00:36:08] And by the way, when they go to a cell that wants cholesterol, they’re going to be unloaded. That’s called dilapidation. When the cells pumped cholesterol out and made the cholesterols bigger, the HDLs bigger, bigger, bigger that’s called lipidation. So, a lipoprotein gaining lipids they lapidate, they become bigger. By the way, what happens to their density when they become bigger? Density is lower. They start floating a little higher. And when they are delipidated, they’re not carrying lipids. Their density goes higher, they sink in the centrifuge tube. I love applying physical chemistry to, I hope it helps people understand some of these lipid mechanics and lipid processes that are occurring.
Cynthia Thurlow: [00:36:51] No. And it’s so interesting, I think a big pearl that you said is if 150 mg/dL for triglycerides is considered to be high, and helping people understand that that’s 75th percentile. We really need to be getting concerned when we see the triglycerides creeping above 100. I usually say 75, but you are more versed in the literature. This is important for people to understand, because just because your total triglycerides or the triglycerides from your lipid panel are showing 140, 130, and you’re probably being told that’s okay. What you’re identifying is we need to get concerned when that triglyceride level is above 100.
Dr. Thomas Dayspring: [00:37:36] Yes. And I’ll give you a pat on the back. If I was going to be totally honest, I said 100 because I totally agree with you. Anything above 70 is not a physiologic triglyceride level. A physiologic triglyceride is about 40 mg/dL, going up to 70 is not going to hurt you too much. But above that, I’m going to tie this all together. If you see a trig between 70 and 150, you at least ought to be thinking, “Am I dealing with early insulin resistance or early ASCVD risk?” And you are, but I have to tell you why the triglycerides really cause atherosclerosis. Because atherosclerosis is the accumulation of cholesterol in your artery wall. It’s not accumulation of triglycerides in your artery wall. But as trigs go up, and we know insulin-resistant people, diabetics get a ton of ASCVD.
[00:38:29] Somehow, the triglyceride must be modifying the particles that are carrying cholesterol that can crash your artery wall. And that’s going to be the final answer to this. And that transformation starts to occur at very low triglyceride levels. You know what’s sad, though, Cynthia? You mentioned you would be told if your trig is 130, you’re normal. And that’s not a sane statement to make. But we actually have and certainly in your experience and in mine, we’ve seen people who go in and have trigs of 300 and are told, “Don’t worry about it.” Oh, my God. [laughs] Look, it’s not all insulin resistance of course, we can inherit genes that affect triglyceride, but almost all of it in the real world is insulin resistance. But you can’t ever dismiss a triglyceride level that is monstrous or even what you are being told because it’s green on a lipid panel. I wish they would get rid of these silly colors or adapt them to the modern. It takes forever for that type of change to occur. But we’re going to tell you as part of our little lipid journey here why you should worry when your trigs are above 75.
Cynthia Thurlow: [00:39:35] It’s interesting, I was with a family member for Christmas, and he was sharing his lipid results, and he was getting ready to go on vacation. And I said, “When you come back, we need to sit down and talk, because I think his triglycerides were 160, his LDL was fairly low, his fasting glucose was in the high 90s.” And I just said, “We need to be doing more than what you’re doing.” And so, I think it’s important for people to understand that there are definitely metrics we want to focus in on at an earlier stage. Unfortunately, the research sometimes takes 10, 15, 20 years to sink into clinical practice. And this is why this conversation is so important, because we’re dealing with a diabetes epidemic and there are far more people that are at risk that really have no idea.
Dr. Thomas Dayspring: [00:40:22] Yeah, you did your brother-in-law a favor there by pointing that out to him. And he should listen to this podcast once you get it up and then obviously come back and consult with you, because that if we put him through an insulin clamp study or even a simpler glucose tolerance test, the man has got serious dysmetabolic issues there. If you think of the markers, you even describe most people know what the metabolic syndrome is. He doesn’t quite meet the criteria there, but you could see he’s on his way to reaching full blown metabolic syndrome. And no doubt that has been sneaking up on him for a decade or two. It’s not like it occurred last week. And for a decade or two, his arteries have been subject to some bad stuff. Takes a long time for atherosclerosis to put us in a graveyard. But if we knew this stuff was happening at an early age, we might ultimately live longer, live healthier, ultimately die of something else. There’s no need to die of ASCVD or dysmetabolic diseases. So, yeah, so you have to learn some of the new numbers there.
Cynthia Thurlow: [00:41:29] If you love this podcast episode, please leave a rating and review, subscribe and tell a friend.



