Ep. 352 Lipid Masterclass: Apo-B Labs and Women’s Heart Health with Dr. Thomas Dayspring
- April 13, 2024
- No Responses
Dr. Thomas Dayspring joins me again today for the third class in our Lipid Masterclass Series. Dr. Dayspring brings a wealth of expertise as a certified specialist in internal medicine and clinical lipidology, holding fellowships with the American College of Physicians and the National Lipid Association.
This hour-long class is devoted to women’s health and abnormal lipids. We continue with our conversation about ApoB, discussing ways to look at other lipid abnormalities related to abnormal ApoBs and talking about our ideal lab values and lifestyle modifications, briefly touching on my lipid journey and the medication I have been taking for the past six months. We examine diagnostics and their limitations, getting into CACs, coronary artery calcification scoring, CIMT, the labs we need to look at, the role of Lp(a), and how it affects our heart. We look into the changes women experience from losing estrogen in menopause, clues women can use to predict future cardiovascular risk, how estrogen helps clear LDL from the body, and the changes occurring with menopause, including higher ApoBs. We also dive into risks women face for cardiovascular disease, the impact of the Women’s Health Initiative study, and absorption and synthesis challenges with cholesterol.
Stay tuned for more!
“If we discover high Lp(a), we are certainly worried about your atherosclerotic future, especially if you get it early on in life, somebody had better be watching that aortic valve closely.”
– Dr. Thomas Dayspring
IN THIS EPISODE YOU WILL LEARN
- Why ApoB testing for inherited lipoprotein disorders is essential
- Why hypo beta lipoproteins (HDL) are critical for maintaining good health
- The benefits of a holistic approach to treating high cholesterol
- The three stages of prevention for atherosclerosis
- How Lp(a) impacts heart health
- The importance of assessing early heart function through Lp(a) testing
- How your pregnancy history can help in predicting your risk for cardiovascular disease
- Why should women be more concerned about cardiovascular disease than breast cancer?
- How the Women’s Health Initiative led gynecologists to be more cautious about prescribing HRT
- How genetically mediated cholesterol abnormalities can impact our ability to absorb and synthesize cholesterol
Bio:
Thomas Dayspring MD is a Fellow of both the American College of Physicians and the National Lipid Association and is certified in internal medicine and clinical lipidology. After practicing in New Jersey for 37 years, in 2012, he moved to Virginia to serve as an educational director for a nonprofit cardiovascular foundation until mid-2019 as a Chief Academic Advisor for two major CV laboratories. Since then, he has served as a virtual cardiovascular / lipidology educator. Career-wise he has given over 4000 domestic (in all 50 states) and several international lectures, including over 600 CME programs on atherothrombosis, lipids/lipoproteins (and their treatment), vascular biology, biomarker testing, and women’s cardiovascular issues. He has authored several manuscripts and lipid textbook chapters and performed several podcasts. For several years, he was an Associate Editor of the Journal of Clinical Lipidology. He was the recipient of the 2011 National Lipid Association’s Presidents Award for services to clinical lipidology and the 2023 Foundation of NLA Clinician/Educator Award. He has over 34K followers on his educational Twitter (X) feed (@Drlipid). He has Gold Heart Member status as a professional member of the American Heart Association, and he serves as a Social Media Ambassador for the European Atherosclerosis Society and the National Lipid Association.
Connect with Cynthia Thurlow
- Follow on Twitter
- Check out Cynthia’s website
- Submit your questions to support@cynthiathurlow.com
Connect with Dr. Thomas Dayspring
Transcript
Cynthia Thurlow: [00:00:03] Welcome to Everyday Wellness podcast. I’m your host, Nurse Practitioner, Cynthia Thurlow. This podcast is designed to educate, empower and inspire you to achieve your health and wellness goals. My goal and intent is to provide you with the best content and conversations from leaders in the health and wellness industry each week and impact over a million lives.
[00:00:30] This is the third episode in the Lipid Masterclass Forum. Today, I’m again joined by Dr. Thomas Dayspring, who is a fellow of both the American College of Physicians and the National Lipid Association and is certified in internal Medicine and Clinical Lipidology.
[00:00:46] Today, we continued our conversation about ways to look at other lipid abnormalities as they pertain to abnormal ApoBs, the lab values that we are striving for, the role of lifestyle modifications, my own lipid journey that I briefly touch on, including the medication I’ve been taking for the past six months, the role of diagnostics and the limitations including discussions around CACS, coronary artery calcification scoring, CIMT, specific labs to look at the role of Lp(a) and the impact it has on our heart, including calcifying the aortic valves, changes with the loss of estrogen and menopause, clues to look for as a woman to predict future cardiovascular risk including things like gestational diabetes, preeclampsia, miscarriages, preterm babies versus full-term babies, early or late start of menses, among many others, how estrogen helps clear LDL on the body and the changes with menopause including having higher ApoBs, risks in women specific to cardiovascular disease, the impact of the Women’s Health Initiative study as well as absorption and synthesis challenges with cholesterol.
[00:02:10] I know you will find this conversation incredibly interesting. This is a full hour-long episode really devoted to women’s health and abnormal lipids. Again, this is the third in a series on the Lipid Masterclass with Dr. Dayspring.
[00:02:33] And so kind of getting back to the ApoB, especially for people, if they’re listening, men or women, and they want to be their own best advocates, what are the lab values we’re looking for someone who is metabolically healthy, no diabetes, no vascular disease, what number are we aiming for versus someone who has known vascular disease or diabetes?
Dr. Thomas Dayspring: Yes, that’s crucial criteria there, because whatever ApoB or whatever level I’m going to recommend to you obviously depends on your baseline risk. If you’re a total nightmare, if you come walking in with a scar on your chest or you’ve had three stents, I’m going to want to turn you into an infant again with an ApoB at 30. But that’s not you and you’re just a middle age, a woman going through menopausal transition, you don’t have coronary artery disease that you know of. And at a certain point, we actually start screening for that nowadays too with noninvasive imaging that is available to us, but a poor tool earlier in life, because what you see in an older person might not be there in a younger person. So, you got to be careful who you’re doing imaging on.
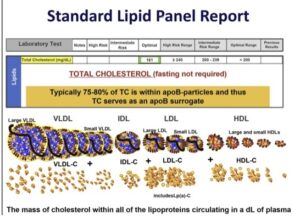
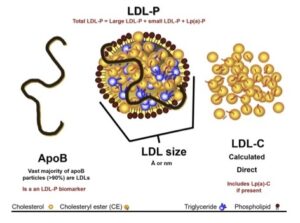
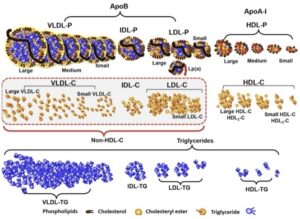
[00:03:39] So somebody comes in, and obviously, they don’t know what a cardiologist is. They’ve never been admitted to the CCU or the bypass unit. They don’t have xanthelasma in their eyelids or sticking out of their elbows, which are cholesterol collections, suggesting a serious genetic cause. For whatever reason, they had a lipid profile. They probably even didn’t do ApoB. But if you listen to us today, you know the things in a lipid panel that ought to jump out at you and make you think you need an ApoB is total cholesterol being high, it’s LDL cholesterol and ApoB particle, it primarily drives total cholesterol.
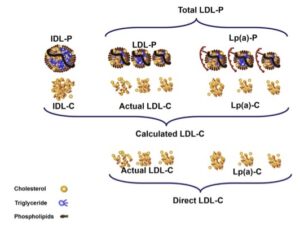
[00:04:15] If you calculate VLDL cholesterol and that’s high, you know you have a triglyceride problem, which always translates to an ApoB problem. So, a triglyceride above 70, as Cynthia said, ought to make you think, I want an ApoB before I say, “I don’t worry about a trig of 110.” And, of course, LDL cholesterol, if it’s beyond a certain level, I would tell you that level ought to be 70 mg, the guidelines would tell you 100, but I would tell you 70. If your LDL cholesterol is 76, I think you ought to be doing an ApoB level.
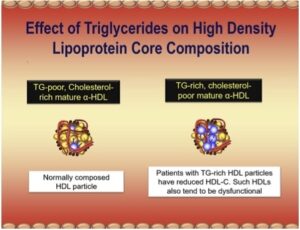
[00:04:47] And of course, the HDL cholesterol, the only way that might, if it’s low, you absolutely need an ApoB level. But we’re actually finding now the old mantra that the higher your HDL cholesterol, the better, is true in some people and not true in others. And women tend to have higher HDL cholesterol than men for reasons we’re probably going to explain. But if a woman comes to me and says, “My doctor did the lipid panel, and yes, my LDL-C is high, and there’s some other bad stuff here, but my HDL-C was 150, so I don’t have to worry about anything.” [Cynthia laughs] My head starts to explode because we know I introduced to you, there are people who have dysfunctional HDLs. They don’t do the good stuff they’re supposed to.
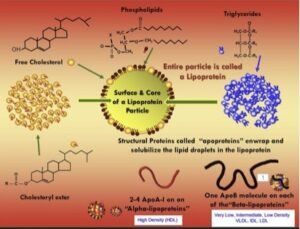
[00:05:28] And in some people, overloaded HDL particles, full of cholesterol, devoid of ApoE, which are not good HDLs, so that would be a person that you’d worry about. So how would you solve it? I’d do an ApoB. I can’t solve the H– but if the ApoB is high, I can take care of that. So, there’s one other test. We didn’t talk about it and I know at some point we will. It’s an inherited lipoprotein disorder called lipoprotein (a). It’s an LDL particle that, attached to the ApoB is another usurper protein called apoprotein (a), small case a, it’s a nightmare atherosclerotic lipoprotein. 1/5 Americans has inherited it, 1/3 blacks, 1/3 Asian Americans, so that has to be part of your initial screening.
[00:06:18] So, the person I’m going to give you ApoB now also had an Lp(a) test, and it’s negative, because we would want a lower ApoB if I knew you had high Lp(a). So, you come in, your lipid numbers maybe are a little out of whack, but they don’t cross. They’re not red on your lipid panel. It comes back from the lab. But if you’ve listened to us today, “All right, I went out and got the ApoB, here’s my ApoB, now what do I worry about?”
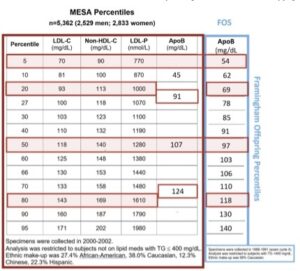
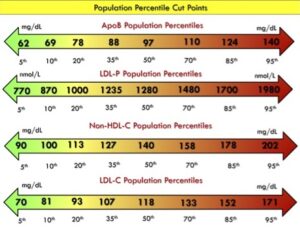
[00:06:43] So, here’s how we look at this, and I’ll send to Cynthia. I don’t know if she does slide notes, but I’ll give you a nice chart that shows all this, that’ll be there for everybody to see. At what point do the ApoB particles have the potential to start crossing your artery wall? We make this judgment if we take regular populations and theoretically, they’re healthy, and we’re excluding the people with coronary artery disease, and we look at what we call population percentiles. So, you could have the lowest levels in the world, and you’d be down at the fifth percentile, that means only 5% of people would have a better reading than you, 95% would have a worse reading. We could look at the ninetieth percentile and say, “Oh, my God, you’re worse than 90% of the people in the world,” not good. We could look at the fiftieth percentile, where you would say, “Well, half are worse than me, but half are better.” Trust me with ApoB, you don’t want to live at the fiftieth percentile because that’s Russian roulette, some will get bad, some won’t.
[00:07:41] So we normally, with lipid concentrations like to see the lipid parameter that you’re looking, you be in the bottom twentieth percentile. That’s usually– And if you could stay there, your chances of maybe some ApoB particles will get in over time, but not enough to give you serious atherosclerosis unless there’s other things going on, high blood pressure, you’re a smoker, blah, blah, blah. We’re talking about healthy people here who don’t have those issues.
[00:08:11] If you really wanted to have a phenomenal ApoB, there is a set of people that for whatever reason, they either catabolize their ApoB particles or they don’t make many. They wind up with very low ApoB or LDL cholesterol levels. It’s called hypobetalipoproteinemia. And if you study them genetically through mendelian randomization studies or if you even follow some of these people over time, they have extremely low incidence of atherosclerosis, if not, no atherosclerosis.
[00:08:41] So, that’s defined pretty much as an LDL cholesterol under 40 to 50, an ApoB under 40 to 50. So, if I could snap my fingers and give everybody in the world an ApoB of 40 or 50, I would. But in most people, you just can’t get there without pharmacologic though. I don’t want to put the world on statins or any other lipid problem right now to make them hypobetas. I just want to maybe get them to the twentieth percentile, and I’ll follow them over time, and if it stays there and they don’t start smoking or their BP doesn’t go out of whack and their menopausal transition isn’t too nightmarish to screw up the lipids and lipoproteins, you’d be happy with that. You can start looking at other diseases that are going to impair either health span or God forbid longevity. And that’s why I say, with the women, I like the whole body. I look at it. But even in men, and there’s a lot of parts– Men’s brains are sometimes important too, so we also look at that and they have certain things below the belt that you want to keep working also. So, there are many things to figure out, and both genders get cancer, so you have to start screening appropriately for that.
[00:09:45] So if I wanted everybody’s ApoB to be in the twentieth percentile, it’s really 80 mg/dL would be fine. But if I really wanted you at the fifth percentile, which is a little bit of a hypobeta, but it’s close, and that would be a level of 60, I think in most healthy people, that’s pretty much overkill, unless you’re reading some longevity book and they know that these hypobetas just don’t– So, make yourself hypobeta, but that’s probably, if you’re otherwise leading a healthy life, going to require drugs to drop an ApoB that high.
[00:10:21] So, if your ApoB is 80, you’re at the twentieth percentile. If it’s above that’s the time where you bring in somebody who’s schooled in nutrition and in lifestyle, and they start going over you with proper exercise programs, proper eating programs, and then you can keep your ApoB 80. And if it’s 90, just doing those things is probably going to make it 80 where I don’t have to take out the prescription pad. Even at a certain point where your lifestyle didn’t do it, there might be some, not many, but supplemental recommendations I could make that at least might reduce the absorption of cholesterol into the body, which should help ApoB a little bit, so you should know about those.
[00:11:07] And ultimately, if your ApoB is not budging because you did the great lifestyle or it’s at a really– You come to me with an ApoB of 120, unless you’re a total pig out nutritionally, you might need a drug. It all depends on your age and how much willing you’re willing to cooperate with the lifestyle and everything. And if your insulin resistance lifestyle works like magic, that’s for sure. So, at a certain point, you’re going to need a drug, but you don’t need a drug day one, if you’re otherwise healthy and your ApoB is even a little scary. Look, even if it was in the eightieth percentile, which I’m thinking, ultimately, I’m going to need a drug. I would like to give you the time to show lifestyle– How low can you get it with lifestyle? maybe I need less drug, or I don’t need two or three drugs to get you the goal. So, I never, never want to downplay lifestyle.
[00:11:51] I have a gigantic Twitter following. People assault me, “Oh, you’re just a drug pusher.” No, you got to realize, I’m a lipidologist, I see the nightmares of the world, and in general, they need drugs. But I think people need appropriate advice with pharmacological care, and they sure as hell need appropriate lifestyle, whatever you want to call it, nutritional and exercise, mental health advice review, perhaps you’re taking other medications for other serious conditions, some of them can [unintelligible 00:12:21] with lipids, so, I have to know a lot about you. So, it’s a complicated decision, but early on– The population we’re talking about now, it’s not drugs.
[00:12:30] Yes if you come in with a crack in your sternum or three stents, if you’re not already on drugs, you’re been going to an incompetent, so I’ll be putting you on. But even if you went to the surgeon or sometimes they’re a little not as aggressive with ApoB as they should be for people with coronary disease. So, I’m probably going to give you further pharmacologic advice, but that’s for the nightmare population.
Cynthia Thurlow: [00:12:52] No, I think this is so important because you’re really stressing how important lifestyle is, number one. Number two, you can get a patient to a certain point, and then considering pharmacotherapy is completely appropriate. And for full disclosure to my listeners, I don’t think I’ve talked about it on the podcast. There’s a genetic predisposition. I am insulin sensitive. I exercise, I sleep well, I’m on HRT, I do all the right things, and I still required medication because– And thankfully, you’re sitting as I say this, my ApoB was 130, this is absolutely a genetically mediated piece. I just had labs drawn last week, so we’re going to see the net impact. I’m on a drug called Zetia, it’s expensive. We very strongly believe that I’m a hyper absorber, which contributes that. But we’ll see where the numbers are. But I’ve been on that for several months now.
[00:13:39] Now, if someone comes to you, let’s say, hypothetically, their ApoB is high, you want to screen them. The screening tests that you’ve been talking about, I’m sure you’re talking about a CAC, so a coronary artery calcification, maybe looking at the specialized carotid artery scans. Are you doing stress testing? Is it really dependent on if someone’s symptomatic or asymptomatic? What are the next steps? Because I’m sure for you, it’s looking a little deeper to figure out what else may be at play.
Dr. Thomas Dayspring: [00:14:07] Sure. Look, it’s a complex evaluation. This is not something in 30 seconds, I can tell you everything you need to know. Chances are we will need additional diagnostic studies for sure. Talk about stress testing, look, if you have an asymptomatic person. Unless they tell you, I’m going to climb Mount Everest next month or something, okay, you want to see what their exercise capacity maybe want a VO2 max for a fancy stress test, but just a plain stress test looking for EKG changes, you have to have serious coronary disease for them to show up. Hey, a nuclear stress test will pick up, but it’s a lot of radiation with a nuclear stress test, so I’m not a big advocate of those for asymptomatic people.
[00:14:47] Nowadays, we do have the coronary calcium, which is a cheap test, looking for calcium deposits, radio-opaque, in your coronary arteries. Not that expensive, widely available, but it’s not good in the younger years, unless you have FH, who you expect heart disease when they’re 16 years old. You are healthy person coming in at 20, 30, even premenopausal, coronary calcium is– If you come back with a 0, nice, but that doesn’t mean anything, you still could have a lot.
[00:15:16] The carotid imaging is certainly the type of imaging you can use in a younger person, but a big caveat. You need to go to somebody who’s well-schooled with carotid intimal thickening analyses. Half of the practices that have them in their office, they don’t know what they’re doing, so you get idiotic readings out, and you’re going to make some serious decisions based on these. I think you’ve got to go someplace that really knows what they’re doing with carotid intimal– So, again, you got to do your homework to see where you’re going.
[00:15:42] There are vascular test flow mediated dilation in other ways where they put blood pressure cuffs, but not everybody is doing them. Again, you have to go to a trusted practice that is well experienced with them and has a long history of doing them. They can all give you worldly clues that your arterial bed is not what it should be or so. So, that’s it, you pretty much– I divide this nowadays. I have a nice slide. When you’re born, those kids we talked about, their ApoB level is normal. And for most kids, throughout infancy and even early adolescence, their ApoB is normal, that’s called primordial prevention. Yeah, you’ll do the odd ball lipid tests, they don’t need them every year at that age, but you don’t see an abnormality, you’re not going to do anything unless the kid is overweight or blah, blah, blah in which case, those tests would probably be abnormal.
[00:16:31] But at a certain point, the ApoB starts to cross those thresholds I talked to, but they haven’t had coronary disease yet. You probably wouldn’t find it. I mean, if you autopsied the kid, you’d find fatty streaks in the aorta. We first found that out in the early studies where kids were getting hit by cars or run over by trains, and at eight years old, they had fatty streaks in their aorta, and we knew atherogenesis occurs very early in some people.
[00:16:59] So once the ApoB is high, I call that primary prevention. I got to work on you through lifestyle or whatever to get you back to the primordial prevention levels, and that’s usually pretty amenable to lifestyle, unless you’re like Cynthia, you’ve picked the wrong mom and dads, and you got some bad genes at play. And look, lifestyle, we never want to dismiss it even in her. You can look at her and see she’s doing lifestyle things well, but she’s still reporting a terrible ApoB. So, of course, keep doing all the things to your healthy lifestyle, but here’s what else you need.
[00:17:31] But once, say, Cynthia, if we did say that coronary calcium on her or even a fancier test called a CTA, computed tomography angiography, they’re not sticking catheters up in your heart and injecting dye into the arteries, that’s like pre-bypass stuff. But we would see not only calcium in her arteries, we would see, “Oh, my God. There are some luminal irregularities or even plaque within the wall of the artery.” And that’s what I call secondary prevention.
[00:17:57] In the old days, secondary prevention meant you had a heart attack or stroke. No longer, secondary prevention means we’ve diagnosed atherosclerosis using non-invasive imaging procedures. So, then we know you’re a hell of a lot closer to a rupture that I talked about. Once the rupture occurs or the luminal occlusion occurs, that’s tertiary prevention. If you survive that, we still can prevent the next one with super aggressive therapy. But you’re probably looking at three drugs in those cases. So, these are some of the diagnostic tests you need to weigh.
[00:18:34] But other than the lipid panel, other than just relying on, “Geez my trigs is a little high.” I do think you need, at a certain level, other tests of insulin resistance or so. So, whether that’s going to be a fasting insulin level. If you do that nuclear magnetic resonance testing, the lipoprofile I mentioned, you will start to see certain lipoprotein signatures of insulin resistance. Your LDLs will be small, your VLDLs will be big because they’re packed full of trigs. Your HDLs will be small because they’re being rapidly catabolized because they inherited triglycerides, and actually make, based on about six lipoprotein characteristics, something called an LPIR, lipoprotein insulin resistance score. Zero is you have no insulin resistance, 100 is if you’re not a diabetic yet, you will be next week. And so obviously you want a level well below 50 on there. As you start to approach 50 or going higher, long before even your glucose might go up, we know you have the type of insulin resistance we’re very worried about, super opportune time to get in there and start doing lifestyle.
[00:19:41] Apart from lipid drugs you know the world is full of all these magical fat disappearing drugs nowadays that people sometimes are jumping on a little too soon before lifestyle, but they’re out there now, even fraudulent ones that somebody’s making in their basement. So, God forbid you had to go to a GLP-1 receptor. I think a prescription product would be smarter to use. They’re in short supply. And third-party coverage may not be so good, but there are–
[00:20:09] Insulin resistance is a whole another animal that, yeah, you’re probably going to need some lipid control, but you’re going to need a lot of other stuff, insulin sensitivity control, and you’re probably borderline hypertensive there too, so that’s going to have to be addressed.
[00:20:23] So, you could see how we start with the basic lipid profile and where we might just– All right we got the ApoB, what we do about it depends upon coexisting things. And if you did test for that Lp(a) everybody right now needs it once in their life, earlier rather than later. If that was out of whack, right now, all we can really do is, I want to take your lowering of ApoB to the next level. I surely want it under 60 if you have a high Lp(a). In the future, we may have drugs that address Lp(a) production. They’re in development. They have to pass rigorous testing and safety testing. So, we’ll see when and if they come to the market, not now.
Cynthia Thurlow: Yeah, it’s really interesting, as I was preparing for our discussion today, one of the things that stood out about Lp(a), that I did not actually know is that it actually can invade our aortic valve, so this is one of the valves in the heart, and can contribute to calcific aortic stenosis, which for anyone that’s listening and saying, “What does that mean?” This is quite significant. I saw a lot of patients, especially older patients, that had aortic valve disease, that ended up going on to need to have their valves replaced and/or repaired, but this can be quite significant. And so this is why the screening tool for the Lp(a), is so important, because if you know at 25 or 30 that you’ve got an abnormal Lp(a), you can be doing things then and not waiting until you’re diagnosed with a disease or valvular heart disease or a calcific aortic valve, because that’s quite significant.
Dr. Thomas Dayspring: [00:21:52] It certainly is. So, if we discover high Lp(a), we’re certainly worried about your atherosclerotic future. But especially if you get early in life, somebody better be watching that aortic valve closely. In the old days, I’d put a stethoscope on your chest and I’d hear a systolic– That’s almost too late. Nowadays, we have echocardiograms, and I think periodically, anybody with high Lp(a), needs an echocardiogram here and there. And Cynthia knows better than I. There are other dynamics that come with the echocardiogram that can give you a lot of things about how good is your aortic valve working.
[00:22:25] In my day, we were told, “Oh, every aortic valve, it’s just they were born with a bicuspid valve,” Meaning they had two leaflets instead of three. And now we’re knowing, yes, that’s still a big problem, but Lp(a) is rapidly coming up as the number one or number two cause of aortic stenosis. And the big characteristic of is it’s calcified. Apo(a) has a lot of bad properties, but it’s sort of osteogenic, so it makes white blood cells turn into osteoblasts in your damn aortic valve, and it’s not good to have cement in your aortic valve or bone. Not good, because the aortic valve, for those listening, it is the main valve that blood flows through when it goes from the heart into your aorta and elsewhere, and you can’t have that narrowed, because over time, the muscle pumping, it gets destroyed. You cannot wait till heart failure, because then it almost doesn’t matter what you do, and fortunately we have so many better ways of assessing early heart function nowadays, and the people who know what they’re doing, jumping in much sooner with aortic valve– which can be done through your chest wall, often don’t even have to crack your sternum, which is good. But if you know you have Lp(a)–
[00:23:37] Anybody who’s got a family history, “Yeah there was a lot of aortic valve in my family,” “Good God get your Lp(a) tested.”
Cynthia Thurlow: [00:23:42] And the big takeaway for the Lp(a) unlike some of these other tests, is that it’s a one-time test. Like, I’ve actually set up my teenagers and my husband to have it checked. And I said, “If you’re all within normal limits, great. But if you’re not, then we know we need to do more than what we’re doing.”
Dr. Thomas Dayspring: [00:24:00] One more point on that, when you go through menopause, and ultimately, we will discuss this, loss of estrogen causes an increase in Apo(a) protein production. So, if a woman, whatever her Lp(a) was premenopause, it’s going to go up a little bit after menopause. And most women, the normal Lp(a) is still normal, but it’s just a little higher. But if you happen to be a serious Lp(a), it’s going to go up. I mean, it was serious before, it’s even a little bit more serious. So that’s the one time it can change. You’re starting this–
[00:24:32] Never test it during an infection. It’s an acute phase protein that your liver produces inappropriately because it probably wants your blood to clot when you’re in a disaster. But if you’re in stable shape, the only time we may have to start repeating it is if any of these drugs that lower it work, they may show us. If you’re a nightmare, here’s how much you have to lower it. In those cases, in the future, we will almost surely be repeating Lp(a), right now, we’re not. I don’t know if ultimately, we’ll get into some of the lipid drugs we’re using. There is one available now that can lower Lp(a) little bit, so maybe if you’re on that drug following Lp(a) would be of interest.
Cynthia Thurlow: [00:25:11] Now, we talked a little bit about women in menopause, but in preparation for our discussion, I had heard you on another podcast talking about risk factors for women, things or clues. So, if you’re a woman who’s not gone through menopause, clues about your medical history, and this is specific to pregnancy history, PCOS, etc., that can clue you in that you are probably at higher risk for complications, lipid issues, etc. And this I found really interesting because this is obviously not my area of expertise, but understanding that your age of pregnancy, any complications with your pregnancy. So, if you think preeclampsia is not something that’s a long-term issue, it can be same thing with gestational diabetes. Can you speak to that? Because I’m sure there are listeners that are impacted and may be completely unaware of this issue.
Dr. Thomas Dayspring: [00:26:05] Sure. So, if I was seeing a new patient who knew they were approaching the menopause or even she’s in her early 40s or whatever, even if she’s– I would ask very specific questions at least me to think, “I think you are in early menopause, even though perhaps you haven’t recognized it yet.” Obviously, there are certain symptoms that it’s a no brainer that something’s going on. But the first thing, if you see a middle-aged woman, when you start doing your initial comprehensive history, you have to spend a lot of time on the pregnancy. First of all, yes, at what age did your periods even begin? When you were a teenager or so. Your menarche early or late, that’s important information. Then you would want to know, were you ever pregnant? Well, no. Did you have any miscarriages that counts as a pregnancy too? If so, how many? So, you want to know the gravida para ratio because if spontaneous abortions do portend future cardiovascular risk.
[00:27:05] If they were successful pregnancies, you say, “Okay, any prediabetes during the pregnancy, any hypertension of pregnancy that they had to address? Nobody ever found protein in your urine, did they, when you were pregnant? I know they probably never checked it, but would you happen to know what a triglyceride level was in the second or third trimester?” All clues that will pretend future cardiovascular risk. If I delivered and the son or daughter was fine, “What was the baby’s weight? Was it a premature delivery? Did they have to induce it or did it go to full term? By the way, once junior or junior S was born, did you lactate or did you not?” Very important as far as both for the child and the mom, as far as future cardiovascular risk.
[00:27:53] Now, if she answered yes to any of those and/or others that I haven’t even elucidated, there are very available women’s guidelines with the checklist of things you have to go down, which, if you check them, you know, potential future vascular issues here. And this is so important even for obstetricians to know this stuff nowadays because they’re the ones delivering these kids. The internist is usually not getting involved at that stage of the game unless the woman was a diabetic during pregnancy or something. But presuming she wasn’t, the obstetrician should know, listen, “I’m done. I’ve developed junior, you know what to do now, you got a pediatrician for the kid, but we did see these little bitty risk factors for you. You were a little preeclamptic, you did have subtle hypertension, your glucose.” Any of those that were present, that woman, I mean, I’m looking at her as, “Uh-oh, future cardiac, big-time trouble.” And that just means that you don’t say to that woman who may have had the kid at age 22 when you hit menopause, go see your internist because they’ll work you up. You go see your internist soon and that internist will do some baseline things in you. That internist will be aware of these things that happen during pregnancy, and that internist will follow your cardiometabolic risk factors extremely closely, and probably long before you get to menopause transition, you’re going to need further lifestyle or even pharmacologic advice.
[00:29:24] Waiting to 40 or 50, average age of menopause is like 51, that’s way too damn late for any woman because you’ve given up decades of possible preventative care in that woman. And look, if you’re telling a woman to come in, she can drag her husband along once a year too for a lipid profile or a cardiovascular risk assessment, [Cynthia laughs] because the men are actually, depending on how ugly their metabolic panel is, do get heart attacks sooner in life than the women. So maybe there is something about this estrogen story that we have to get into and why when estrogen goes bye bye at menopause, other issues may evolve.
[00:30:05] A quickie, one of the regulators of that LDL receptor that clear the ApoB particles out of plasma is estrogen, so women lose estrogen at menopause, all of a sudden their LDL receptors are and is as many as they used but they don’t live as long as they used to. So, her ApoB clearance goes up a little bit and ApoB starts to rise. The man never had damn estrogen to begin with, so his LDL receptors are at probably an unhealthy level sooner than they would be in a woman. So that’s one way you relate hormones to atherosclerosis.
Cynthia Thurlow: [00:30:34] No, I find it also fascinating and it’s interesting. I think a lot of women worry about breast cancer, and what we actually need to be more concerned about is cardiovascular disease, ASCVD. And this is from a paper that I just read that it said one in 3.2 deaths in women a year, heart disease is the number one killer, accounting for one death every 80 seconds and HRT, so hormone replacement therapy is a sex specific primary preventative therapy for heart disease and all-cause mortality. So, if you’re not talking to your doctor, your NP, your PA about HRT, and you’re in perimenopause or menopause, you should be, because more women are impacted by heart disease than the breast cancer. I’m not saying breast cancer is not important to be concerned about. I’m just saying from a loving place, from someone who spent 16 years in cardiology, there were far more women who presented late. They present atypically, they put it off because they’re worried about taking care of everyone else, and yet this is what’s more than likely going to kill us.
Dr. Thomas Dayspring: [00:31:34] I’m so full of jokes. I graduated med school in 1972, my postgraduate training in another three years, and then I went into private practice. So, through med school and residency program, “Don’t worry about women. The heart attacks are all the men who get them and stuff.” I used to scratch my head because I loved hanging in the CCU. They were just being invented in my day. And it was like, “If you were smart, that’s where you wanted to hang out because you had a chance to maybe save a few,” but there were women in the CCU. “What the hell are they telling me? Women can’t get heart attacks?” Now some of them were smokers, yes, but still, not all of them were, so women get heart attacks.
[00:32:12] And you see these stats where, yes, ASCVD is the biggest killer of women and men, and everybody thinks, “Yeah, it’s our great grandmothers who are dying of these heart attacks.” Yeah, some of them, that’s true. But if they actually live that long, they’re probably going to die someday. You don’t want to see the modern stats of even premenopausal women who are getting cardiac, ischemic, or obstructive atherosclerotic disease or nonischemic coronary disease, which is a vasospastic issue that women– So you just get that out of your head that women don’t get atherosclerosis. They do. And like everything else, guys and gals, the sooner we develop it.
[00:32:52] The estrogen story is so interesting at the early part of my life, you were a jerk if you didn’t start every woman on estrogen including super high-dose estrogen. In my early days, what’s a progestin? We didn’t even know about that. And so that started to evolve that. Well, we certainly have to give progestins and maybe at a certain point we could lower the dose of estrogen, because even with the oral contraceptives in those days, we’re seeing strokes in young women because they drown those young women.
[00:33:20] The first, they will cease the estrogen doses were ridiculous. So that all got tempered out and rediscovered over time. But then it was, if you’re a gynecologist, every woman was going to be put on hormone therapy as she approached menopause, no exceptions to the rule, unless there was a blatant contraindication, not Factor V Deficiency, blah, blah, blah. Little bit of breast cancer started to emerge, early on there wasn’t even that big a worry. And all of a sudden, these estrogen studies started to come out. The first was the HERS study, where in John Hopkins they actually took women with pretty serious coronary disease, and they gave them the most popular product used. It was Prempro at the time, conjugated equine estrogens and hydroxyprogesterone acetate, on the belief that giving these women hormone therapy would erase their coronary artery disease. And of course it didn’t. It’s actually a null study, some women did have some adversity at the end, so, oh, my God, and what’s, the newspapers, estrogen is killing women. They don’t tell you it was women with pretty serious heart disease, which would now pretty much be a contraindication to most hormonal therapies.
[00:34:32] So that was the first study that came out, but then ongoing, was the Women’s Health Initiative, which was a gigantic study. But some women who were perimenopausal, early menopausal, and a lot of them were late menopausal women, which we now know is probably not the woman you’re going to start on, but these women either got a placebo or they got HRT. Again, Prempro, if they didn’t have a uterus, they got just Premarin without the hydroxyprogesterone.
[00:35:04] And lo and behold, as they started to crunch the numbers before the paper even got published, it came out that, again, there might be a bad cardiac signal. But remember, you’re looking at a diverse population of women, including grandmas, early menopausal, and not even yet menopausal women, but on their way. So, it’s tough to know if you’re giving women to this diverse population. Was estrogen hurting one group and perhaps helping the other group, that didn’t come out early on.
[00:35:32] But the newspapers, oh, my God, it was all over TV, “Stop estrogen doctors, you’re killing women.” And the MPA, CEE, there was maybe a little breast cancer signal there. Nobody was looking at the intensity of that signal or what was the real risk. But the headlines were nightmarish. So, HRT prescriptions were pretty high over a few years. Even gynecologists were prescribing a lot less HRT. And you know why that was not good? Because as we now know, there are some women who can get nice benefit from appropriate types of hormone replacement therapy, and there are some women who should never get it for God’s sakes. We’re a little smarter now. We always are. As blips come in medicine, we always react, and ultimately it filters out, but it took a good 15 years of more post hoc analysis of these trials to see. So now the indication is pretty much perimenopausal, early menopause, unless there’s a reason not to use it, appropriate menopausal hormone therapy if that’s what you want to call it, is probably doing good.
[00:35:42] There always is a dilemma then at what stage? Should I go on forever? Should I stop it? And that’s not an easy decision to make. But again, if a 75-year-old woman is walking in, I’m probably not starting her. This even applies to not only heart disease, it applies to bone, where you really want to get estrogen in early. Yes, we have other osteoporotic therapies, but in my day, it was the bisphosphonate. We drowned women with them, and it took us five to ten years to find out, “Oh, my God, you’re creating brittle bones.” In some women, you’re killing too many damn osteoblasts, you don’t want to kill it or osteoclasts. You need osteoclasts for proper bone remodeling. So that was another lesson we had to learn.
[00:37:22] And then, of course, the anabolic drugs got developed, and we have so many more products nowadays. But that’s a complex thing that has to be evaluated in a woman. Pelvic things is I’m not going to put you, per se, on oral estrogen to help your vaginal wall or your prolapse, the bladder or so, that’s going to be localized estrogen therapy. So again, it’s another hole. Even no matter what, you’re a woman who needs estrogen therapy, is it unopposed? Is it opposed? If it’s opposed, are you going to use– Progestogens is the natural progesterone, plus a ton of synthetic products called progestins. So, with estrogen, which progestogen do I want to recommend? And if I do recommend it, at what points in the cycle or is it intermittent? It’s very complex how to figure out.
[00:38:15] And even now, when it gets to the estrogen, there not only are many different estrogen products, I prefer estradiol, which is what the ovary makes. But do I give it orally? Do I spray it? Do I rub it on her? Do I stick a high dose in her vaginal vault? so you could see and how many do you believe, I will tell you, no intern is going to residencies giving any education on the complexities I just– Gynecologists might be, I would hope so, but they’re not given any education on ApoB or how do I worry about the heart in a woman or what woman would I not give estrogen because of the heart. What about Lp(a) and that’s very controversial too, should you give estrogen to that or not.
[00:38:54] So you can see, we’re right back to what Cynthia and I told you. How does a woman get good care nowadays? How do you find a physician that knows everything like that? So, look, I think you got to go to the National or it’s now called the Menopause Society, not the North– They would have people who are certified in that. Probably a good choice. Certainly, if you know you have an ApoB problem or for sure an Lp(a) problem, you might want to look out somebody certified in lipid.
[00:39:25] And by the way, they’re not all MDs. There are nurse practitioners, there are physician assistants, there are osteopaths and a naturopath. Osteopaths are really the same as an MD, but we all have different types of training and interest. At your stage in a game, you should know what your problems are and you got to find the right person. But you don’t have to be an MD per se.
Cynthia Thurlow: [00:39:46] Yeah, no, I think you bring up so many good points and I endeavor, and my mission with this podcast is being able to deliver the best and the brightest in the healthcare and wellness space so that it can allow people to become more empowered and inspired. And I agree with you. I’ve been through multiple providers to find the person I’m with now that listens to me.
[00:40:09] He’s a male, he’s an MD. He listens to me. We make decisions together. He’s very respectful of my needs. He also challenges me when he doesn’t agree with an opinion I have. And so, I think everyone deserves to have really good care. And to your point about HRT and finding out what mode of HRT does someone need, not everyone in perimenopause and menopause needs the same things.
[00:40:32] As an example, some people need progesterone just around their cycle and their luteal phase. I’m certainly a proponent of progesterone. I think that’s made such a big difference in my sleep. But in terms of looking at other things that can contribute to abnormalities and lipids, I want to make sure before we end the conversation today, because obviously we’ll have another one. I was jokingly telling Dr. Dayspring I had eight pages front and back of prep which says a lot because there’s so many different directions to go down. But something that I thought was really interesting, and I’ve learned a lot listening to you and learning about your work. When we’re talking about cholesterol abnormalities, things that are genetically mediated, people can either be absorbing too much cholesterol, I’m going to oversimplify or they can synthesize too much cholesterol.
[00:41:20] So before we end our conversation today, let’s tie this in so that people are aware that the primary mechanism that may not be working optimally in their body could be like it is for me. I have an absorption problem. I absorb too much cholesterol and that drives a lot of the issues, along with an abnormal ApoB, let me be clear. But can we touch on that subject just to kind of tie up our conversation today? And obviously, I’ll bring you back, because we have so many other things we could talk about, including medications and other labs that we can be looking at.
Dr. Thomas Dayspring: [00:41:52] Yeah, she’s touching a topic dear to my heart, prejudice. [Cynthia laughs] But I think most lipidologists would tell you the best textbook in the world that deals with lipid therapy is called Therapeutic Lipidology. It’s a thick hard covered book. First came out in issue one. Now issue two this year was produced. And if you get asked to write a chapter in that book, somebody thinks you know something about something in lipids. And in both of those books, I wrote the chapter on how the body handles sterols, specifically absorption and synthesis of sterols. And I’ve already told you yes, its cholesterol, but there are a lot of other sterols and what do you have to know about them? So, it’s a topic so dear to my heart.
[00:42:32] I also worked in biomedical laboratories, super advanced cardiovascular for seven years. And of course, they get into all the advanced type of clinical chemistry that you can do. And that’s where I even added to my expertise in understanding absorption of sterols, because we’re doing these types of tests that can be done on hundreds of thousands of people. And obviously I had to study that and learn to it, talk to experts in the field about it. So, I fell into menopausal medicine first, but then I dumped into the absorption synthesis. And how cool is it that actually I wrote the paper, we were the first one to discover menopausal women start hyper-absorbing cholesterol, wow, it fit in perfectly.
[00:43:16] And we’re going to need another podcast to [Cynthia laughs] really get into the depths of cholesterol absorption. And what could go wrong, either genetically or even in a menopausal woman to do that. With that aside, I just wanted to wet your appetite that it’s such a crucial topic, again, that most clinicians just have never been taught. So, unless they’re self-taught, or going to reading my chapters in the book, or going to CME courses, they’re never going to learn it.
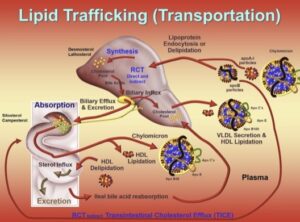
[00:43:44] We want to have normal ApoB. So, if you have a high ApoB, we have to instruct your liver either stop making ApoB particles or God darn it upregulate those LDL receptors that grab those ApoB particles and clear them. Because if the liver clears them, they get destroyed. And every ApoB particle you destroy is one less that can go in your artery wall. So, the liver is the master controller of peripheral lipid control. Again, forget the brain, that’s different. Your brain is not connected to the intestine with respect to sterols, although maybe with other things it is, I’m learning in some of these microbiome discussions.
[00:44:20] But anyway, so I have to if Cynthia comes to me with a high ApoB, two things, I have to try and find out why she has a high ApoB. And if I really discover that, I think I could probably make a much smarter treatment decision on how to lower ApoB in her. So, it’s what makes a liver stop making LDL receptors, so it stops clearing ApoB, LDL particles, one, the liver is either synthesizing too much cholesterol or it’s not, but the intestine is absorbing too much cholesterol and the chylomicrons are grabbing it all and dumping it in the liver, overloading the liver with absorbed cholesterol.
[00:45:03] Look, cholesterol toxicity in the liver is one of the causes of fatty liver. So, if the liver is getting a lot of intestinally delivered cholesterol, I’m not making LDL receptors. I sure as hell don’t want to pull in LDLs carrying more cholesterol so they don’t manufacture. And there are what we call nuclear transcription factors in the liver that tell your genes what enzymes and what proteins and what receptors to make or not make. So, if Cynthia has something wrong with her intestine, that it is over absorbing cholesterol, she’s drowning her liver and cholesterol, she’s making less LDL receptors. So obviously, if I knew that ahead of time, I would say, “Cynthia, I think we’d probably have to work on reducing the absorption of cholesterol in you. Number one, I want to have a little discussion with you, so you understand this is not a simple process. It’s regulated by a few things.” And once you understand that, then either the lifestyle or pharmacologic therapies and some of them may be an intestinal supplement, you’re going to be much more prepared to say, “You know, you make a good point and I’ll try it and see.” Ultimately, the bottom line is going to be, if we addressed absorption, did her ApoB go down? Because there are other things affecting those LDL receptors apart from synthesis and absorption that could be if she inherited a goofy gene that’s affecting her LDL receptors and you throw hyperabsorption on top of that, that’s why you approach pretty scary ApoB levels, so, who knows?
[00:46:31] But at least the initial therapy in her would be, let’s reduce absorption. She did mention she’s taking a pill, Ezetimibe is the generic, the brand name is Zetia, but the generic is much more affordable. It’s a simple one a day pill with very few side effects. We can include you in on them, but they’re like next to nothing. And you would significantly reduce the amount of cholesterol in her intestines because it screws up that receptor that is pulling in cholesterol, deactivates it in part. So, you’re going to absorb less cholesterol. Your chylos are going to deliver less cholesterol to the liver. All of a sudden, the liver needs cholesterol to make bile acids, so it will upregulate more LDL receptors and clear more ApoB particles. And that is exactly how Ezetimibe reduces ApoB. There will be a little bit less production when the liver makes VLDLs and LDLs, there’ll be less cholesterol going into them. So, it’s also working on this ApoB particle synthesis route, but also the clearance. And clearance is the primary way of getting rid of those.
[00:47:32] And this is just so fascinating because that receptor that pulls cholesterol from your gut lumen into the intestine, which makes it way to your liver, your liver has that same receptor that sits at the hepatobiliary interface where the liver interacts with your biliary system, which is how bile acids and cholesterol get to the gut. But that receptor can also pull cholesterol back out of your bile into the darn liver, oh no. But the same drug, Zetia, that blocks the receptor in the gut also blocks it at the– So, most people don’t know, Zetia/Ezetimibe works in two crucial interfaces to reduce the amount of cholesterol getting into your body. So that’s the short man’s absorption story.
Cynthia Thurlow: [00:48:15] If you love this podcast episode, please leave a rating and review. Subscribe and tell a friend.



