Ep. 368 Lipid Masterclass: Exploring Insulin Resistance, Statins, and Alternatives with Dr. Thomas Dayspring
- June 8, 2024
- No Responses

I am thrilled to present the last class of our Lipid Masterclass series today with the esteemed Dr. Thomas Dayspring. Dr. Dayspring is board-certified in internal medicine and clinical lipidology and is a fellow of the American College of Physicians and the National Lipid Association.
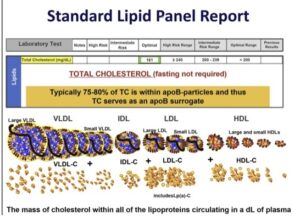
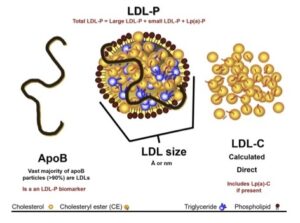
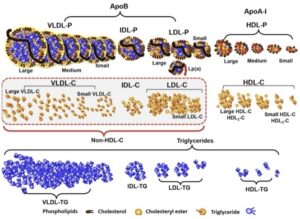
Today, we round things out by diving into medications for lipid abnormalities and discussing lipid physiology, with Dr. Dayspring shedding light on insulin resistance and statins and cautioning against statin use for those predisposed to diabetes or insulin resistance. He also explains why LDL particle size is not worth testing and discusses ways to identify specific laboratory abnormalities.
Be sure to stay tuned for the AMA session to follow, where Dr. Dayspring will answer listeners’ questions.
It has been a privilege engaging with Dr. Dayspring throughout this masterclass series. I know you will have learned a lot from it!
“We deal with a lot more small LDLs than we do bigger because insulin resistance and diabetes are so prevalent in our world.”
– Dr. Thomas Dayspring
IN THIS EPISODE YOU WILL LEARN:
- The lack of research and consistency in addressing the needs of women in various stages of life
- Dr. Dayspring discusses the use of bile acid sequestrants for lowering LDL cholesterol
- Dr. Dayspring discusses the history of bile acid sequestrant use, explaining why their use is limited
- How bempedoic acid and statins lower LDL cholesterol
- Potential contraindications for bempedoic acid
- The benefits and risks of using fibrates to reduce heart attacks
- Dr. Dayspring explains why fibrates work best for genetic hypertriglyceridemia
- Why reducing ApoB is essential for atherosclerosis patients, especially for high-risk patients
- Dr. Dayspring explains why small LDL particles are dangerous
- The ideal ApoB level for those who have no heart disease and are not diabetic
Bio:
Thomas Dayspring MD is a Fellow of both the American College of Physicians and the National Lipid Association and is certified in internal medicine and clinical lipidology. After practicing in New Jersey for 37 years, in 2012, he moved to Virginia to serve as an educational director for a nonprofit cardiovascular foundation until mid-2019 as a Chief Academic Advisor for two major CV laboratories. Since then, he has served as a virtual cardiovascular / lipidology educator. Career-wise, he has given over 4000 domestic (in all 50 states) and several international lectures, including over 600 CME programs on atherothrombosis, lipids/lipoproteins (and their treatment), vascular biology, biomarker testing, and women’s cardiovascular issues. He has authored several manuscripts and lipid textbook chapters and performed several podcasts. For several years, he was an Associate Editor of the Journal of Clinical Lipidology. He received the 2011 National Lipid Association’s Presidents Award for services to clinical lipidology and the 2023 Foundation of NLA Clinician/Educator Award. He has over 34K followers on his educational Twitter (X) feed (@Drlipid). He has Gold Heart Member status as a professional member of the American Heart Association, and he serves as a Social Media Ambassador for the European Atherosclerosis Society and the National Lipid Association.
Connect with Cynthia Thurlow
- Follow on Twitter
- Check out Cynthia’s website
- Submit your questions to support@cynthiathurlow.com
Connect with Dr. Thomas Dayspring

Transcript
Cynthia Thurlow: [00:00:02] Welcome to Everyday Wellness podcast. I’m your host, Nurse Practitioner Cynthia Thurlow. This podcast is designed to educate, empower, and inspire you to achieve your health and wellness goals. My goal and intent is to provide you with the best content and conversations from leaders in the health and wellness industry each week and impact over a million lives.
[00:00:30] This is the fifth podcast in a Lipid Series Masterclass with the amazing esteemed Dr. Thomas Dayspring. As I’ve mentioned before, he’s a fellow with both the American College of Physicians and the National Lipid Association and is double board-certified internal medicine and clinical lipidology.
[00:00:49] Today, we round out the conversation talking about medications for lipid abnormalities as well as a bit of lipid physiology. These included bile acid sequestrants, bempedoic acid, statins, fibrates, Zetia, omega-3s, and PCSK9 inhibitors. We spoke about the role of insulin resistance and statins and why this is probably not a fantastic drug if someone is already diabetic or insulin resistant. And lastly, we spoke about why LDL particle size is largely irrelevant and is not worth testing, and ways to look out for specific lab abnormalities.
[00:01:36] Again, this is the last, the fifth in a series of lipid masterclasses. Stay tuned for the AMA format that I will do with Dr. Dayspring answering all of your questions. It has been such an honor connecting with him, and I know you will have found these five podcasts incredibly valuable, not just for yourself, but for your loved ones.
[00:02:01] We’ve kind of touched around, talked around some of the medications that we can utilize. And I’m thinking back to like old school bile acid sequestrants, like Welchol that we did use probably in the early 2000s. We were still using that to some degree, things that are generic and unfortunately, the big issue with bile acid sequestrants is you have to use quite a bit of pills to be able to get the net effect. When you were still providing care to menopausal women, we’re using much Welchol. Can we talk a little bit about some of the effects of Welchol? Because actually some of the questions that came in, there are some people that are taking Welchol, surprisingly. It’s not a bad drug. It’s just you need a lot of it [chuckles] to get it to work.
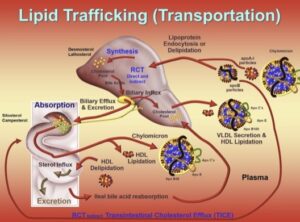
Dr. Thomas Dayspring: [00:02:42] Look, the greatest trivia question in lipidology is, “Name the first drug that passed a randomized, blinded, empowered trial showing it could reduce atherosclerotic events.” And it was in 1984 and it was the Lipid Research Clinic trial. And they use an early sequestration called Cholestyramine. Welchol came a little later on. It’s actually an improved type of bile acid sequestration, or bile acid polymer, as they like to call it.
[00:03:13] But look how it worked is those drugs bind up bile acids in your gut. Normally, your ileum reabsorbs all your bile acids and the liver reuses them. If your bile acid sequestration is binding bile acids, they don’t get reabsorbed at the ileum. The liver has to start using up liver cholesterol to make new bile acids. And if the liver uses bile cholesterol up, the liver will grow more LDL receptors, which clear your ApoB particles, so that’s how they work.
[00:03:43] Remember, this is before we had anything. So, reduction was dose dependent. If you use a little bit, you didn’t get much. If you drown somebody with it, you could get a 20%, 30% reduction, most people in between there. The problem was with the Cholestyramine. It was like putting sand in a glass of orange juice. It was not fun to take, lot of bloating, a lot of constipation. So, to be honest with you, look, I had to use them [chuckles] because there was nothing else. Only people who had survived heart attacks and knew they were on life’s last limb were compliant with long term use of it.
[00:04:18] Now, once, Welchol came along, it was a little less adversarial to the gastrointestinal tract. So, you could take it. Same thing, you had to take large amounts of it, several scoops a day in liquid. They actually developed a liquid form that you could drink for people who didn’t want to do that, and you still had the same efficacy as the old-time bile acid sequestrants.
[00:04:40] As we started using Welchol, we found out, “Geez, in our diabetics, the sugars are doing better.” So, they actually did further studies and Welchol has an FDA indication to improve glycemic control in the diabetic. And look, we know why, it’s way beyond today’s podcast, but it’s kind of interesting. You have a lipid lowering drug that was also beneficial to glucose. And remember, we’re talking back in the era when we didn’t have a lot of stuff. Even the things were using for glucose then weren’t the most wonderful. We didn’t have the GLP-1 receptor agonist, and we were tiptoeing into the Metformin and lot of sulfonylureas which was a big mistake. So, bile acid sequestrants didn’t. I love giving these aside, because they knew that blocking bile salt reabsorption would lower LDL cholesterol. It’s called, the POSCH trial. They remove people’s ileums, and if you remove the ileum surgically, you can’t reabsorb bile acids. And actually, they did an outcome trial, and it reduced heart attacks and improved LDL cholesterol.
Cynthia Thurlow: [00:05:45] It’s a bit extreme. [laughs]
Dr. Thomas Dayspring: [00:05:47] Yeah. And it was way back when we didn’t have six other drugs. [laughs] But good luck today telling, I always joke, patients who say that, “I’m not using any of these drugs.” “All right, we could take out your ileum,” [laughs] to see if they go for that, but it works, and it just was proof of concept that the ileum is part of our lipid homeostasis. So that’s a factoid you might need to pass the lipid boards one day you’ll never for anything else.
[00:06:10] So, the bile acid sequestrants were the first drugs. They cannot be used anymore because of the side effects. The one place they still are used a little bit, they are totally non-systemic. They are not absorbed. They do nothing to the– So, a pregnant women with familial hypercholesterolemia are often still given Welchol to use in that circumstance. They’ve actually evolved into, we could probably still use statins in those women or so, but you have to be going to an expert who knows what they’re doing. But the old, they have the X category with statins. They don’t use those categories anymore. But now it’s pretty much left up to your judgment. Probably shouldn’t do it if you’re not a lipidologist, well experienced in treating pregnant women. But if you have a woman with FH who’s already had coronary disease or something, benefit versus risk, you might want to try it, certainly past the first trimester. We don’t really use them that much anymore because there’s just so many other choices. But I do want you to know, it’s not ezetimibe, it’s not blocking cholesterol absorption. It’s blocking bile salt reabsorption, so people confuse the two. So, Welchol with Zetia actually is a good combination therapy if for some reason you don’t want to take any other lipid drug, and there are trials showing the efficacy with those two together. But again, Welchol is Welchol.
[laughter]
Cynthia Thurlow: [00:07:34] I think that the one thing I learned the biggest takeaway was constipation was not most people’s friend. And so, if I couldn’t get patients up to six a day, we would have to pivot and think about alternatives for sure. Now, you’ve mentioned bempedoic acid. Now this is one of the new kids on the block. You mentioned it’s a pro drug, it’s active in the liver. Talk to us about how this works mechanistically. What does it do to the LDL receptors? Is it particularly effective for ApoB, etc.?
Dr. Thomas Dayspring: [00:08:05] Sure. Remember, what gives you more LDL receptors, which enhances clearance of ApoB particles, is the liver either has to manufacture more LDL receptors or you have to extend the half-life of those LDL receptors, that’s the PCSK9s. But any of the drugs we use that deplete the hepatic pool of cholesterol by inhibiting synthesis, so that’s going to be a statin or bempedoic acid or by inhibiting absorption and delivery of cholesterol to the liver, that would be ezetimibe, upregulates LDL receptors, and they all reduce ApoB, usually in a dose dependent fashion, except bempedoic acid is only one dose and as is ezetimibe right now, unless you want to go off label statins as we’ve talked about, you could keep titrating to get more LDL receptors if you want.
[00:08:54] So anything that depletes the pool of cholesterol in the liver will improve clearance of ApoB particles. So, remember this fancy cholesterol synthesis thing that we talked about to start off the podcast? It’s actually 37 steps. And step one is citric acid becoming acetyl-CoA, which in two more steps becomes mevalonic acid. So bempedoic acid inhibits step one of cholesterol synthesis. The rate limiting step in cholesterol synthesis is step three, and that is catalyzed by an enzyme called HMG-CoA reductase, which is what statins inhibit to variable degrees, some statins inhibit it more than others. So, since that’s the rate limiting step of cholesterol synthesis, statins are most potent synthesis inhibitor on lowering ApoB or LDL cholesterol. Bempedoic acid which takes out step one, will reduce cholesterol synthesis, but not to the same degree that a statin will. But hey, if you go on bempedoic acid, at the end of the day, you’re synthesizing less cholesterol in the liver and your liver will say, “I need cholesterol to make bile acid.” So, your liver will express more LDL receptors. So, bempedoic acid lowers ApoB, LDL cholesterol, non-HDL cholesterol.
[00:10:09] Now, the typical statin is going to give you– Again, it’s always dose dependent, but let’s say 30% lowering or so. You want to go up to the gorilla statins, you can get higher. Bempedoic acid by itself is around 15% to 20%. Remember, both bempedoic acid and statins are more efficacious if you happen to know the patient is a hyper-synthesizer as opposed to a hypo-synthesizer. Ezetimibe monotherapy across the board 15% if you’re lucky, 20% ApoB, LDL cholesterol lowering, more if that happens to be a hyper-absorber of cholesterol, less if they’re a hypo-absorber. So that being said, we now have outcome data with bempedoic acid monotherapy. So that degree of ApoB lowering will reduce X amount of heart attacks be it in a primary or secondary prevention setting.
[00:11:03] Now, its FDA indications when it came out, “All right, you could add it to a statin in people with FH where the statin didn’t get you to go, or if they had familial hypercholesterolemia, that would be an indication to add bempedoic, because the statins just are not going to get you there.” Very recently, because of their outcome data, they got indications to, “Hey, if you have a statin intolerant patient,” because the trial they did that reduced outcomes, you couldn’t be on a statin because these were people who just had severe statin intolerance. So bempedoic acid monotherapy works, so it tells you the drug works. And actually, event reduction was pretty close to some of the early statin event reduction. So, it’s probably a good drug, but again, you’re not going to get approval for that unless a statin has failed, you have documented, you can’t take a statin or you have FH, blah, blah, blah. That’s the problem. It’s a $6000 a year drug, maybe a little less, but that’s beyond most people to do that. But it’s a great drug.
[00:12:02] It inhibits the enzyme that’s involved in that conversion of citric acid to acetyl-CoA, is only expressed in the liver. So bempedoic acid will not reduce cholesterol synthesis in your brain, in your eyeball, in your muscles, blah, blah. And one of the advantages to it is they just don’t see the muscle aches with bempedoic acid that they, of course, have seen with statins. So, the other thing you know statins, there’s a slightly increased incidence of diabetes, especially in people with underlying insulin resistance. With bempedoic acid, not only is there no aggravation of insulin resistance or glycemia, there’s actually a little bit of improvement. And that’s because there’s another pathway by inhibiting that enzyme, it goes through AMPK. And it’s very complicated. Almost certainly in the future, it may be a longevity drug, it may be a hypertriglyceridemia drug.
[00:12:56] There’s a lot of other things they have to do if the drug company wants to spend the money to do those investigations. But on paper, you can make a great case that this could be a miracle drug. Right now, it’s a helpful drug and helping control ApoB, if you can get it. So that’s all you really have to know. But this is a great and you can probably get coverage nowadays in a high-risk patient who just can’t take a statin. So, they’ve loosened up their indications a little bit based on the recent trial.
Cynthia Thurlow: [00:13:26] Yeah. And it’s interesting, I guess, the contraindications that I read, because, of course, I went down that rabbit hole, was looking at patients that have gout, nephrolithiasis, I haven’t said that word in a long time, kidney stones. And then there was a 1% increase in gallstones. Did you see that in your–
Dr. Thomas Dayspring: [00:13:41] No. Well, the studies have reported that.
Cynthia Thurlow: [00:13:43] Yeah.
Dr. Thomas Dayspring: [00:13:44] And look, if you even do deep reading on ezetimibe, there’s a little bit of a perhaps increased risk of gallstones. Remember, Zetia is affecting your biliary concentrations of bile acids and cholesterol. And the oddball patient, you might slightly create a lithogenic bile. But the incidence is so low, I don’t even know if you have to inform a patient about that ahead of time. Maybe you should, because they might google it. As somebody who’s had their gallbladder out, you don’t even until it’s an overnight stay in the hospital [unintelligible 00:14:14] with the laparoscopic techniques nowadays, and you don’t need your gallbladder for anything, you’re not screwing up anything because you’re not storing bile anymore.
[00:14:23] But the uric acid is interesting. And therefore, if you have a patient who’s had episodes of gout, uric acid nephrolithiasis. Not all nephrolithiasis is uric acid, but if you happen to know that you can get trivial elevations in uric acid. It interferes with one of the metabolites of oxidative degradation of uric acid. So, what they tell you is, obviously, if somebody’s had a lot of gout, it’s probably not the lipid drug you want to use or maybe if their baseline uric acid is in the stratosphere, you might want to take care of that first with some allopurinol or something and get– So, it’s one of these relative contraindications. So, in the extreme cases, you wouldn’t go there, but say you come in and you’re a borderline uric acid, could you use bempedoic acid if you have to? Yes. Obviously, you would advise the patient, “If you get a swollen toe, call me up, or a knee swelling and we’ll keep an eye on your uric acid on subsequent blood tests,” usually it’s not going to go up that much to cause a problem. If you thought it was a worry, you could start the patient on allopurinol first and get the uric acid well controlled, and therefore you wouldn’t have a lot of worries with the bempedoic acid. But it is important to know that that’s for sure. And look, if you’re a doc and you’re prescribing any drug for the first time, please read the package insert, and it would be clearly outlined to you what measures to take. So, it’s not a total contraindication, but there are warnings there for it with that.
Cynthia Thurlow: [00:15:57] Yeah. And it’s interesting–
Dr. Thomas Dayspring: [00:15:58] The gallstones would be the same with it. Like, I don’t know. I’ll deal with it if it happens. I think I can reduce heart attacks significantly. And when you look at benefit versus risk, gallstones versus reducing heart attacks, I think the benefits outweigh the risks.
Cynthia Thurlow: [00:16:15] Oh, absolutely. And then, there are a couple more that kind of blew it on my radar, old school fibrates. Does anyone even still prescribe them anymore? I used quite a bit of Tricor years ago and Lopid.
Dr. Thomas Dayspring: [00:16:28] Yeah. The Welchol was the first drug in a randomized, blinded clinical trial to reduce heart attacks. The second was a fibrate. And there are actually a couple of trials, the Helsinki Heart Trial and the VA-HIT Trial, but it was fibrate monotherapy with a fibrate called gemfibrozil. Back in the branded day, it was Lopid, now you can get it generically. And of course, there have been subsequent fibrates manufactured in the fenofibrate class.
[00:16:56] So as a monotherapy, gemfibrozil worked as good as any statin did in a trial. Helsinki with primary prevention, VA-HIT with secondary prevention. So, nobody would use a fibrate first line anymore, because we have drugs that are so much better. And gemfibrozil is a bad news fibrate because it is absolutely contraindicated with statins. It interferes with the catabolism of statins. You get very high statin levels and rhabdomyolysis as a problem. They actually had to take one statin off the market. Cerivastatin was sold as Baycol back in the day because the manufacturer was pushing doctors, “Use the highest dose of Baycol.” And people were combining it with gemfibrozil and bad news, actually the pharmaceutical company took it off the market. But so, if you’re going to use gemfibrozil for whatever reason, don’t combine it with a statin.
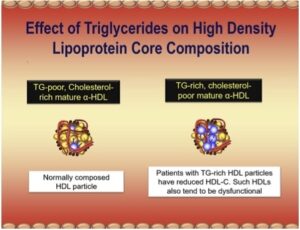
[00:17:46] Look, fenofibrate carries the same contraindication with a statin, except if you read the literature, totally different. It does not interfere with the enzymes that gemfibrozil screwed up statins with but the FDA, “Hey, a fibrate is a fibrate,” so it’s in their book on that. So feno would still be a contraindication, but we could do except there have been now a couple of trials combining fenofibrate with statins looking at MACE, Major Adverse Cardiology Events and it didn’t work. So, I don’t think you should be combining a fibrate with a statin. Here’s the one place you should be using a fibrate. And it would be a minority of your patients, those who come in with triglyceride levels well above 400, 500. That’s a genetic cause of hypertriglyceridemia. That is not diabetes causing trig. It might be diabetes aggravating a genetic problem. So, fibrates are actually your best drug there. You would likely be combining them with high-dose omega-3 products, because when you have trigs in the thousands, it’s tough to get them down to– And you want to get them below 400 or 500 because you take pancreatitis out of the picture. So that’s pretty much where fibrates have been relegated to severe genetic hypertriglyceridemia nowadays.
[00:19:03] The one reason we used to like to use the fibrates is because we thought they all had remnant particles, and they do. When your trigs go up, you have small LDLs, your LDL-P is off the chart, your ApoB is off the chart, but these potentially atherogenic chylomicron and VLDL remnants are off the chart. Good news, statins, ezetimibe, bempedoic acid, and PCSK9 inhibitors all remove remnant lipoproteins, so you don’t need fibrates anymore to get rid of remnants.
Cynthia Thurlow: [00:19:33] It’s really exciting, especially looking at these PSCK9s when I was reading about them in prep for our second conversation, just realizing it may not be available to everyone to utilize them. But in many instances, it’s interesting for those that are high risk or have that familial susceptibility, this is a really exciting drug. In reading and reviewing the literature, who are the like ideal circumstances, obviously high-risk atherosclerosis, probably the familial dyslipidemia-related issues, but where do you see it being most efficacious?
Dr. Thomas Dayspring: [00:20:05] Yeah, listen, as a true believer that you got to make ApoB as low as possible, especially in your high-risk patients. So, anybody with existing atherosclerosis, whether they’ve had an event or not, and we have imaging ways to ascertain how much atherosclerosis you have. FH is defined as you have an LDL cholesterol above 190, you could go and do the genetic testing if you want, but most people with FH, you’re not going to find the darn gene because it’s polygenic. There’s a lot of genes, and unless you’re doing full genome analysis, you’re not going to get all of those. So, an LDL-C above 190, that you cannot get to go with a statin or a statin ezetimibe. Now it’s 190 in adults, it’s 140 in kids. So, remember, kids have that. So, anything above 140 in a kid is FH until proven otherwise. So, that’s the ApoB road we go down as clinicians is statin, statin ezetimibe, hey, you got bempedoic acid, you got PCSK9, but there are obviously third-party payer issues to using them. And if the statin and ezetimibe doesn’t get you where you got to go, then you have to make your case to the third-party payer. Easier said than done sometimes. [laughs]
Cynthia Thurlow: [00:21:19] Oh yeah.
Dr. Thomas Dayspring: [00:21:20] But that’s your algorithm right now.
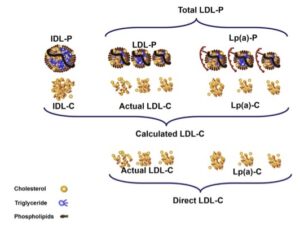
Cynthia Thurlow: [00:21:23] Yeah. And last question I had for you, when we spoke on our last conversation a lot about labs and testing to be asking for. I don’t think we spoke most much about particle size. Does that even play into your risk factor stratification for your patients? Do you think that it’s falling out of vogue, if you will, in comparison to some of these other lab tests that we have talked about?
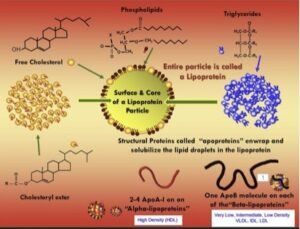
Dr. Thomas Dayspring: [00:21:49] Well, it’s an interesting topic, but it’s nothing anybody should be measuring or making any decisions on. So, listen, LDLs are a heterogeneous grouping of LDL particles from more buoyant to less buoyant. As they lose lipids, they become less buoyant, they become more dense. So, you’ve heard the term small dense LDL. Any small LDL is dense by definition. Any dense LDL is small by definition. It’s a redundant use of two adjectives, but regardless. On the other side of the heterogeneous family, you have the more buoyant, larger LDL particles, and why are they larger? Because they carry more lipids.
[00:22:25] Now, typically, an LDL is going to be carrying cholesterol, but if you had a triglyceride rich LDL, it would be big and buoyant also, so does it matter? Well, here’s where it matters. How does the LDL receptor remove LDL particles? It grabs ApoB, but it’s only looking to grab a very small segment of the ApoB peptide and that is called the LDL receptor binding domain.
[00:22:51] Now, if you have LDLs, come in big, small, but also normal size right in the middle. So, on a normal size LDL, the ApoB has a certain confirmation that exposes the LDL receptor binding domain, and LDL receptors really clear normal size LDLs well. If your LDL is small, or conversely if it is big, the ApoB on the surface gets distorted. All of a sudden, the LDL receptor binding domain might not be as visible to the LDL receptor. So, there is decreased clearance of both big LDLs and small LDLs. And that’s why people with small LDLs, that’s one of the reason they have very high LDL particle counts, but it’s the same with big LDLs. Do people with familial hypercholesterolemia have big LDLs, have high ApoB levels? They sure do, because of clearance issues.
[00:23:45] So, the other thing that deal with a lot more small LDLs than we do bigger, because insulin resistance and diabetes is so prevalent in our world, and that’s a triglyceride world, the trig pretty much above 80 or 120. The trigs are going to get into the LDL particles where they never should be. And if trigs invade an LDL particle, hepatic lipase takes out the trig, and the particle gets smaller, and the small particle doesn’t bind as well to the LDL receptor. So, the plasma resonance time of the small LDL is ghost for several days. So virtually anybody with small LDLs who’s not on a lipid modulating drug will have a very high LDL particle, counter ApoB.
[00:24:30] You show me the study, the person who has small LDLs but has a normal ApoB, impossible. So, is the small LDL dangerous because it’s small or because they can’t be cleared and it sends ApoB through the roof, and you got so many LDL particles? Yes, most of them small. They’re just crashing your artery. But it’s the same with the big damn LDL particle, it can’t get cleared, and that’s why people with FH get so much coronary disease. The big balloons are crashing your artery walls.
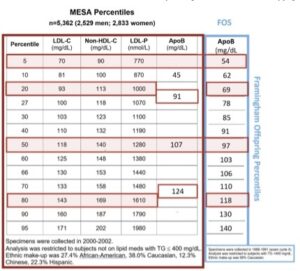
[00:25:01] I can send you, and maybe for your slide notes on this right from the MESA studies that big LDLs have decreased clearance, small LDLs have decreased clearance, and normal size LDLs do not. This was discovered way back in the 1990s with Fredrickson, Levy, and Lees. So, it was a handy gimmick for people doing lab tests, “Oh, you got to find the small LDLs.” Now, you just have to find a high ApoB. And the same drugs that you use to clear small LDLs will clear big LDLs. And of course, you’ve got to throw lifestyle on top of it. Perhaps even more important if they have the small LDLs, because they’re the insulin resistant hypertriglyceridemic patients. So, not a slice does it matter.
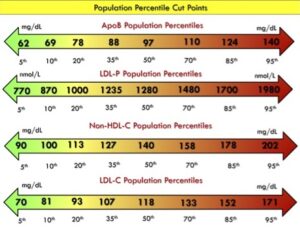
Cynthia Thurlow: [00:25:39] No, I think this is really important and this is a big pearl. We need to focus more on that ApoB, because irrespective of the particle size, it’s irrelevant if that ApoB is outside the norm. And let me reiterate, in case anyone has forgotten from our previous discussions, we want that ApoB less than 80 in patients that are not diabetic and with heart disease. So, if you’re a non-diabetic, no heart disease, less than 80. If you have diabetes, you have vascular disease, you are diabetic, you want it less than 60. Everyone should be having this tested without question.
[00:26:13] Dr. Dayspring it has been such an enormous honor and privilege to connect with you, not once, but twice. Please let my listeners know how to connect with you outside of this podcast, how to be invested. You have tremendous content on Twitter, you’re active on LinkedIn, how to connect with you if they have questions or want to learn more about your work.
Dr. Thomas Dayspring: [00:26:33] And indeed, they are the best two ways. I am, as you said, very active on Twitter. If you have a question, maybe it’s something I’ve addressed. Maybe it’s something you want addressed. If you measure, if you voice your questions civilly, and I read into it, you want to learn. I answer a lot of tweets. If you want to be obnoxious and tell me I’m an idiot or cholesterol doesn’t matter, you’re probably not going to get a nice response from me or you’ll certainly get muted because I can’t be bothered with– LinkedIn is pretty much I’ll only accept you as if you’re a professional, so I don’t have laymen contacting me on LinkedIn that much. But I’m very good at answering tweets, so that’s the best way and happy to do it because there’s so much to teach about this. I love doing these podcasts with people like Cynthia. I’m an old man here. I’m not going to be around forever, so I have to keep teaching, teaching, teaching these young kids like Cynthia. She’s a kid in my mind.
Cynthia Thurlow: [00:27:33] Aww. Well, thank you. I appreciate that. But for listeners to know that not only after this podcast series comes out, we will do a separate podcast where Dr. Dayspring and I will do some Q&A. We’re not going to be providing medical advice, but we can definitely be providing some information that you can utilize to take to your healthcare practitioner team and advocate for yourself.
[00:27:53] If you love this podcast episode, please leave a rating and review, subscribe and tell a friend.



